“Thank you for taking care of me over the past 21 years, giving me the chance to be reborn again and again!”
Sunlight streamed through the windows, dancing on the golden fringe of the silk banner. Mr. Kai (pseudonym), now 57 years old, tightly held the hand of Dr. Xu Jiongyuan, Director of the Third Medical Department at Fuda Cancer Hospital, expressing his heartfelt gratitude.

Defying a Death Sentence
"Stage IV liver cancer at 39 years old... there’s not much we can do..."
Twenty-one years ago, Mr. Kai was diagnosed with liver cancer. Doctors in his hometown told him he only had three to six months to live. He later underwent surgical resection at our hospital, and remarkably, lived in good health for the next 18 years.
In 2022, the cancer recurred. He returned to our hospital for cryoablation and interventional therapy. Afterward, targeted immunotherapy helped stabilize his condition. Earlier this year, signs of recurrence reappeared, prompting another visit to the Third Medical Department. Fortunately, the recurrent lesions have since shrunk, and the remaining active tumor areas have reduced in size and activity—his condition is showing signs of improvement.
Personalized Treatment Plans for Every Challenge
01 Initial Diagnosis
In 2004, Mr. Kai experienced right chest pain and was diagnosed with a 7–10 cm tumor on his liver. The diagnosis shocked the entire family. Determined to seek treatment, Mr. Kai learned about the minimally invasive techniques at Fuda Cancer Hospital and took a 36-hour train ride to Guangzhou with his father. As the pillar of his family, he was willing to sell everything to get treated.
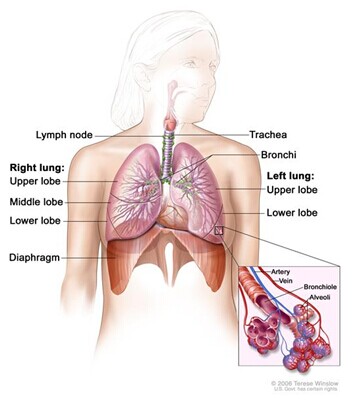
Mr. Kai couldn’t understand how someone as healthy as he was could develop liver cancer. Dr. Xu Jiongyuan explained that it could be related to his long history of hepatitis B. Studies have shown that people infected with the hepatitis B virus are 15–20 times more likely to develop liver cancer than non-infected individuals. Over 80% of liver cancer cases are linked to HBV infection. Because the liver lacks pain nerves, early-stage liver cancer often presents no symptoms and is usually diagnosed in the middle to late stages when surgery may no longer be an option.
Mr. Kai’s tumor was large and wrapped around blood vessels. The medical team recommended interventional therapy first to suppress and shrink the tumor before attempting surgical removal—a strategy known as “conversion therapy,” aimed at turning unresectable advanced liver cancer into a surgically resectable one.
Fortunately, he became a candidate for surgery and successfully had a quarter of his liver removed. Post-surgery, he underwent chemotherapy and interferon therapy, achieving excellent disease control and returning to a normal life and work routine.
02 Recurrence
Eighteen years later, in April 2022, Mr. Kai began experiencing recurrent diarrhea and bloating. He sought help at a local hospital and discovered another liver mass.
“Right lobe of the liver shows an 11.4 × 10.6 × 9.1 cm hyperechoic lesion with irregular shape, unclear margins, and heterogeneous internal echoes; AFP levels reached 4137 ng/ml…”
“I should’ve gone for regular check-ups. I would’ve caught it early and controlled it,” Mr. Kai often said, regretting that his long-term stability had made him complacent, allowing the tumor to grow unnoticed.
He underwent transcatheter arterial chemoembolization (TACE), continuous arterial infusion, and local cryoablation. These treatments stabilized his condition, with his tumor markers steadily decreasing and the liver tumor shrinking. After discharge, he diligently followed medical advice, maintaining immunotherapy with targeted agents and undergoing regular follow-ups in his hometown.

03 Second Recurrence
In February of this year, Mr. Kai’s follow-up revealed a mild increase in AFP. Upon returning to our hospital, imaging showed that most of the recurrent lesion had undergone coagulative and liquefactive necrosis, but the remaining active areas had increased.
After a multidisciplinary team discussion, Mr. Kai underwent intratumoral drug injection and chemical ablation to treat residual tumor tissue. Because the lesion was primarily supplied by the lower right hepatic artery, interventional radiologists performed a super-selective arterial embolization under DSA guidance. Post-embolization imaging showed that the tumor’s blood supply and staining had nearly disappeared.

Currently, the recurrent lesions have slightly shrunk again, with significantly reduced active tumor tissue compared to before.
Every treatment decision was carefully tailored to Mr. Kai’s condition and the latest advancements in cancer care. Treatment goes beyond just killing tumors—it also aims to minimize physical and emotional harm, helping patients maintain their quality of life.
Of course, beyond advanced technology and professional expertise, trust and compassionate care between doctor and patient were also key to Mr. Kai’s recovery.

“When old friends meet again, it’s a special kind of joy. Time flies, and our gray hair bears witness to how we’ve grown old together,” sighed Hospital President Dr. Niu Lizhi when he saw Mr. Kai again.
In the blink of an eye, 21 years have passed. From the anxiety of his first hospitalization to the calm familiarity of his regular visits, Mr. Kai now feels like he’s returning to a warm and loving home every time he comes in. From the friendly greetings and attentive nursing care to advanced treatments, each visit has filled him with confidence and comfort.


Fighting cancer is not just a battle against disease—it’s a long-distance marathon of life, run hand in hand by doctors and patients.
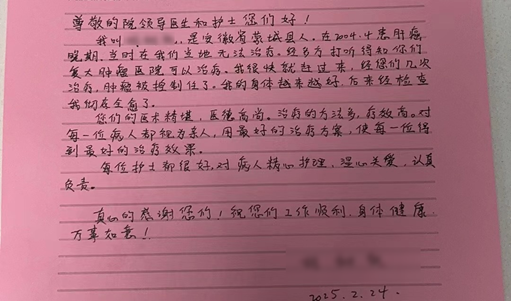
The silk banner embroidered with “Noble Medical Ethics, Heartwarming Compassion, Superb Skills, Known Far and Wide,” and the shaky handwriting of a heartfelt thank-you letter, are the best witnesses to the healing power of humanity in medicine.
Mr. Kai’s optimism and trust give us tremendous motivation, strengthening our resolve to walk this medical journey together, side by side.