There is a “fast track” between the intestines and the liver—the portal vein. Normally, this route helps transport nutrients absorbed from the intestines to the liver. However, once a tumor develops in the colon, this passage can turn into a “highway” for colorectal cancer cells to metastasize to the liver. This was exactly the challenge faced by Uncle Wang (a pseudonym), a man in his 50s.
A Liver Lesion Revealed to Be Colorectal Cancer
In July 2021, Uncle Wang was found to have a liver lesion during a routine physical examination, which was suspected to be a tumor. After further diagnostic work-up, local doctors concluded it was not primary liver cancer but most likely a metastasis from colorectal cancer. A colonoscopy confirmed a 3×3 cm tumor about 18 cm from the anus, diagnosed via biopsy as sigmoid colon cancer.
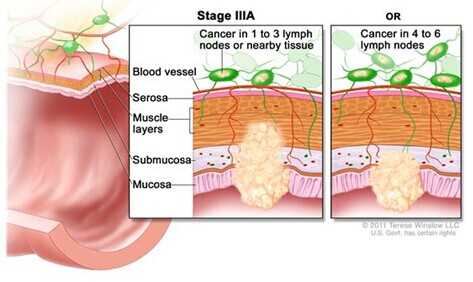
The liver is the most common site for colorectal cancer metastasis. Due to the direct blood flow from the intestines into the portal vein, colorectal cancer frequently spreads to the liver. Around 15–25% of colorectal cancer patients present with synchronous liver metastasis at diagnosis, and another 15–25% may develop metachronous liver metastasis after radical surgery of the primary tumor.
Colorectal cancer often has no symptoms in the early stages or only presents with mild symptoms like bloody stools or irregular bowel movements, which are easy to ignore. Uncle Wang had experienced loose and black stools but, feeling otherwise fine, he didn’t give it much thought—until the test results revealed cancer.
Seeking New Treatments to Alleviate Pain
The local hospital proposed a treatment plan involving chemotherapy followed by surgery. Uncle Wang underwent six months of chemotherapy combined with targeted therapy, which stabilized his condition. In March 2022, he had radical rectal surgery, lymph node dissection, and hepatic tumor resection. Post-operative pathology confirmed metastatic adenocarcinoma in liver segments S4, S5, medial segment, left lateral lobe, and caudate lobe. Tumor regression grade (TRG) was 2, indicating a partial response with residual cancer cells and evident tumor shrinkage.
To consolidate the effect, Uncle Wang received maintenance therapy combining chemotherapy and targeted therapy after surgery. However, in a follow-up in August 2023, liver masses reappeared. He underwent interventional therapy at a local hospital. “It was excruciating!” he recalled. Being pain-sensitive, he was unsatisfied with the treatment. Upon recommendation, he started immunotherapy with targeted drugs.
But by the following year, scans revealed that the liver tumors had enlarged and multiple swollen lymph nodes appeared around the hepatic portal. Uncle Wang, unwilling to endure more painful treatments, began looking for gentler alternatives. After extensive inquiries, he found Fuda Cancer Hospital in Guangzhou and sought treatment at the Fourth Medical Department in September 2024.
Multidisciplinary Strategy: Tackling Cancer One Step at a Time
Upon admission, imaging showed a large metastatic lesion in the right liver lobe measuring 7.4×6.7×9.2 cm and multiple enhanced lymph nodes around the hepatic hilum and retroperitoneum. Given Uncle Wang’s medical history and current status, Dr. Pang Xiaoming from the Fourth Medical Department initiated a multidisciplinary consultation. The proposed treatment plan was to first conduct interventional chemotherapy and embolization to reduce tumor blood supply and shrink its size, followed by cryoablation to relieve tumor burden and control disease progression.
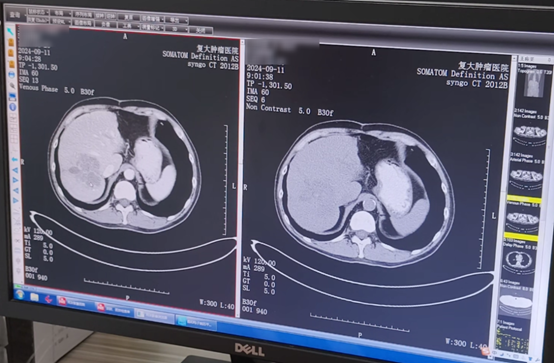
△ CT scan during first admission in September 2024
However, upon hearing the plan involved interventional therapy, Uncle Wang immediately refused. “The last time hurt terribly.” Fearful of reliving the pain, he was reluctant. But after thorough explanation and reassurance from Dr. Pang, he decided to try again.
He underwent hepatic arterial infusion chemotherapy, super-selective embolization of the upper right hepatic artery, and hepatic artery catheter placement, all guided by digital subtraction angiography (DSA) and performed under local anesthesia.
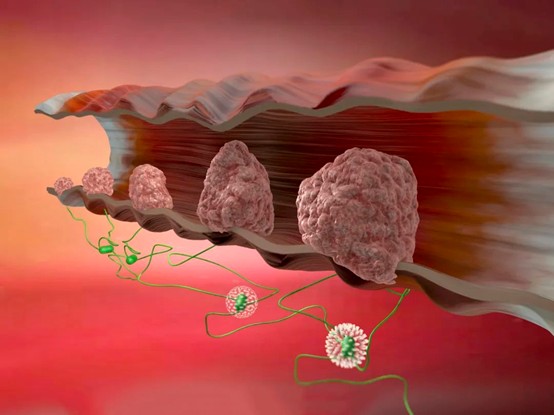
Interventional radiologists accessed the femoral artery and navigated a catheter into the tumor’s feeding artery, where they injected chemotherapy drugs and embolic agents. This not only “poisoned” the cancer cells but also “cut off their food supply,” leading to tumor necrosis from both ischemia and high drug concentration. A microcatheter was then placed in the proper hepatic artery to allow continued chemotherapy infusion in the ward.
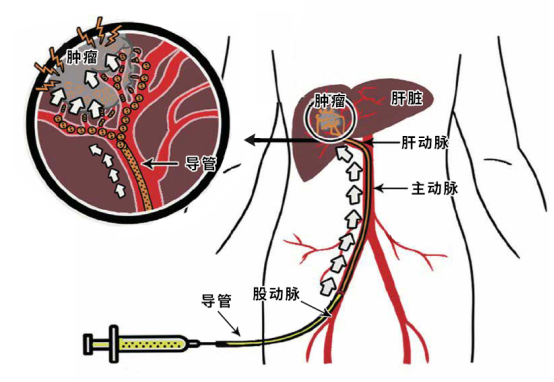
△ Image source: internet
This method avoids the systemic dilution of chemotherapy seen with intravenous administration and bypasses the liver’s “first-pass metabolism,” where drugs are partially broken down before reaching the bloodstream. It also reduces side effects like bone marrow suppression and gastrointestinal reactions, offering minimal trauma, short recovery time, and repeatability.
“I felt great—almost no discomfort, and I could eat and sleep as usual!” A week later, Uncle Wang underwent cryoablation of the liver tumor and continued combined treatment with immunotherapy, targeted therapy, and chemotherapy. By April this year, his follow-up showed that the liver metastases had shrunk and were less active. However, the retroperitoneal lymph nodes had grown larger and more numerous, prompting his return to Fuda.
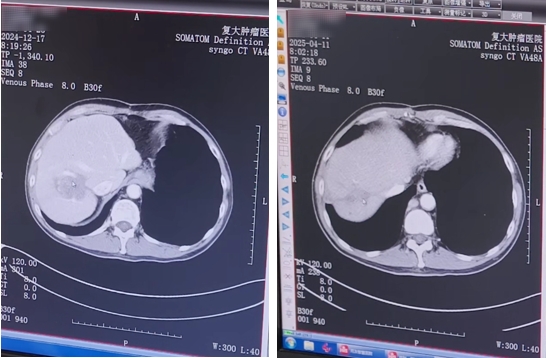
△ Left: December 2024 follow-up; Right: April 2025 follow-up
“This time I had iodine-125 seed implantation.” Though unfamiliar with the treatment, Uncle Wang returned to Fuda without hesitation, reassured by his positive past experience. “The medical staff explained everything clearly before the procedure—what it is and what to expect.” He hopes for even better results this time.


△ Iodine-125 seed implantation therapy
Health Tip: Know More, Stay Healthier
As the saying goes, “Illness enters by the mouth.” Colorectal cancer is largely a lifestyle disease, often nicknamed “a cancer caused by eating.”
During our chat, Uncle Wang admitted to favoring meat, salty and spicy food. Even during treatment, he didn’t strictly control his diet. But many studies now confirm the link between colorectal cancer and eating habits:
Meat-heavy diets: Especially red and processed meats with minimal fruit and vegetable intake. High-fat, high-protein, low-fiber diets create harmful metabolites in the body that irritate the intestinal lining and trigger cancer.
Strong flavors: Spicy, salty, sour, fried, smoked, and grilled food can overstimulate the digestive tract and increase cancer risk. Late-night eating also disrupts digestive rest.
Barbecue and smoked food: These cooking methods can produce carcinogenic compounds like heterocyclic amines, polycyclic aromatic hydrocarbons, and benzopyrene.
Fast food: Popular among young professionals, fast food is calorie-dense but fiber-deficient, increasing colon cancer risk.
Alcohol and smoking: Both are known risk factors. Smoking causes chronic irritation of the colon and rectum, increasing cancer risk.
To avoid being “targeted” by colorectal cancer, one must not only stay active but also “manage the mouth.” This includes reducing red and processed meat, eating more fiber-rich foods, ensuring adequate calcium and vitamin D intake, supplementing with beta-carotene and vitamins, avoiding overly strong flavors, limiting alcohol, and quitting smoking.