When people hear the word “advanced,” many assume it’s a death sentence—especially with widespread metastases. But that’s a misconception rooted in outdated thinking. With the continuous advancement of treatment options and the emergence of highly effective therapies, even “advanced breast cancer” no longer means there’s no hope.

6 Chemotherapy Sessions, 26 Radiotherapy Sessions, but the Tumor Worsened
Sandi (pseudonym), a 43-year-old woman from Indonesia, discovered a lump in her left breast two years ago, occasionally accompanied by pain. Medical examinations revealed a 3 cm mass with a high suspicion of malignancy. Following her local doctor’s advice, she underwent surgery. Post-operative pathology confirmed triple-negative breast cancer, with cancerous spread to the axillary lymph nodes.
To control disease progression, Sandi started intravenous chemotherapy. However, after the first cycle, she discovered she was pregnant and had to pause treatment. In 2024, one month after giving birth, she resumed therapy. Unfortunately, despite 6 cycles of chemotherapy and 26 sessions of radiotherapy, her condition worsened significantly—particularly the sternum area, where she developed a painful and enlarging mass.
She was told, “It’s nothing serious, just take some painkillers.” Dissatisfied with this diagnosis, Sandi traveled to Malaysia for further testing. PET-CT scans revealed widespread metastases throughout the body: bone, pleura, chest wall, subcutaneous scalp, and axillary lymph nodes.
From Chemotherapy Crisis to a Ray of Hope in China
Her first step was another round of chemotherapy. However, Sandi suffered a severe allergic reaction to the drugs. She lost consciousness, experienced heart failure, and had to be rushed to the ICU for emergency care. “I thought I wouldn’t live to see tomorrow,” she said, disheartened and hopeless.
Her husband never gave up. He sought medical advice everywhere, determined to find any chance of hope. Eventually, a glimmer of light appeared in Guangzhou, China. He contacted the Indonesia office of Fuda Cancer Hospital and, after consultation, decided to bring Sandi to Guangzhou for inpatient treatment.
Tumor Shrinks Nearly Half in Just Two Months
On April 13, 2025, Sandi arrived at Fuda’s Medical Department IV in a wheelchair. Her condition was poor. Though she could still get out of bed, she was extremely weak, suffering from chest tightness, shortness of breath, and right leg pain—unable to walk for long without resting. Further tests showed metastases not only in previously identified sites but also in the meninges and liver, along with a pulmonary artery embolism.
Given her high tumor burden and fragile condition—at risk of respiratory depression, worsening pulmonary embolism, and intracranial hemorrhage—Associate Chief Physician Dr. Xing Yanli quickly organized a multidisciplinary team and tailored a personalized treatment plan:
For the pulmonary embolism and urinary tract infection: Symptomatic medication;
For the chest wall mass: Biopsy and cryoablation, which confirmed breast cancer metastasis;
For meningeal metastasis: Gamma Knife therapy was used instead of whole-brain radiotherapy due to her poor physical condition.
During treatment, Dr. Xing noticed Sandi tested positive for Her2 (low expression), meaning she could potentially benefit from ADC (antibody-drug conjugate) therapy. ADCs work by specifically binding to Her2 proteins on cancer cells, delivering cytotoxic agents directly, and triggering immune responses through antibody-dependent mechanisms.
After discussion and evaluation, the team administered ADC therapy combined with immunotherapy and targeted treatment.
To Sandi’s surprise, after just one cycle, visible tumor shrinkage occurred. After two cycles, follow-up scans showed significant reduction—nearly 50%—in the meningeal lesions, chest wall metastases, axillary lymph nodes, and liver tumors, achieving a partial response (PR).
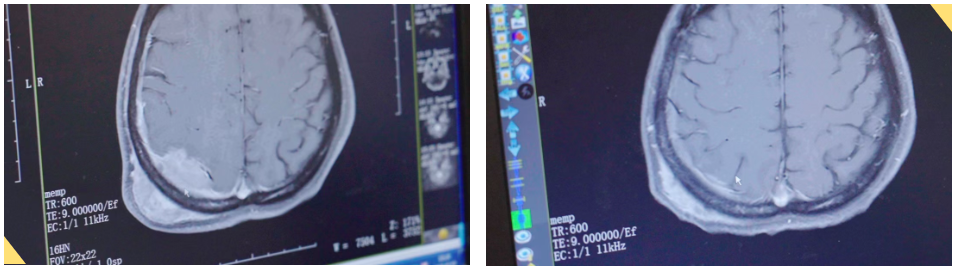
△ Meningeal and subcutaneous metastasis: Before admission (left), after treatment (right)
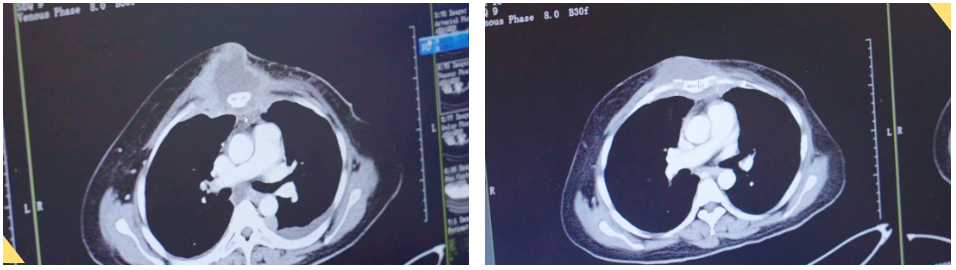
△ Chest wall and sternum metastasis: Before (left), after (right)
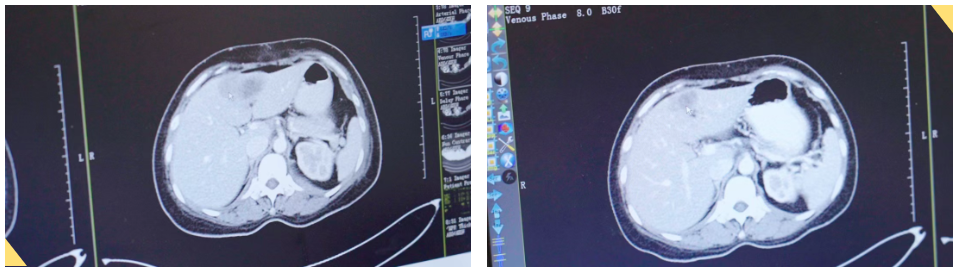
△ Large liver metastasis: Before (left), after (right)
Sandi’s right leg pain disappeared. Her breathing and mobility improved dramatically—she no longer needed a wheelchair. “Thank God, thank Fuda!” she exclaimed. She deeply appreciated the professionalism and compassion of the medical team and now hopes to maintain her health and enjoy life to the fullest.
Cryoablation and NanoKnife: Cutting-Edge Tools in Precision Medicine
Sandi’s case is a successful example of combining cryoablation with Gamma Knife therapy, highlighting the vast potential of precision oncology in treating solid tumors. Fuda Cancer Hospital, one of the pioneers in multidisciplinary cancer care in China, continues to push the boundaries of patient outcomes using cryoablation and NanoKnife (IRE) technologies.
Cryoablation: A Minimally Invasive Freeze Against Cancer
Cryoablation inserts a probe into the tumor under image guidance. Using ultra-low temperatures (typically -140°C to -160°C), it freezes and destroys cancer cells within 15 minutes. This forms intracellular ice crystals, causing cell dehydration, membrane rupture, and cell death.
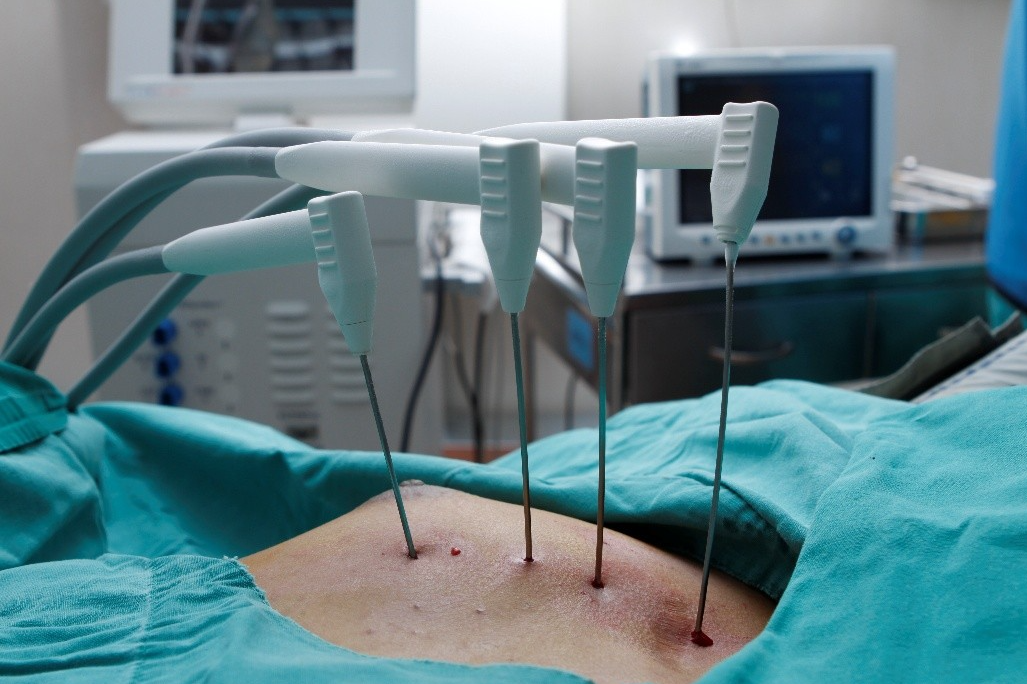
At Fuda, “visualized cryoablation” allows real-time monitoring of the ice ball to ensure complete tumor coverage while protecting nearby nerves and vessels. In Sandi’s case, her 5 cm chest wall mass was ablated with just two tiny punctures, leaving only small, rice-grain-sized scars.
Moreover, Fuda has been researching the immune-activating effects of cryoablation. Tumor antigens released from frozen cancer cells can stimulate the body’s immune response. A multicenter study at Fuda found that combining cryoablation with immune checkpoint inhibitors improved 3-year progression-free survival by 17% compared to ablation alone.
NanoKnife: Non-Thermal, Precision Ablation
NanoKnife (Irreversible Electroporation, IRE) delivers high-voltage pulses (1500–2500 volts) that last only 100 nanoseconds, creating nano-scale pores in cancer cell membranes. This causes cells to leak and die—without generating heat. Thus, it avoids damaging heat-sensitive structures like blood vessels and bile ducts, making it ideal for tumors near vital structures.
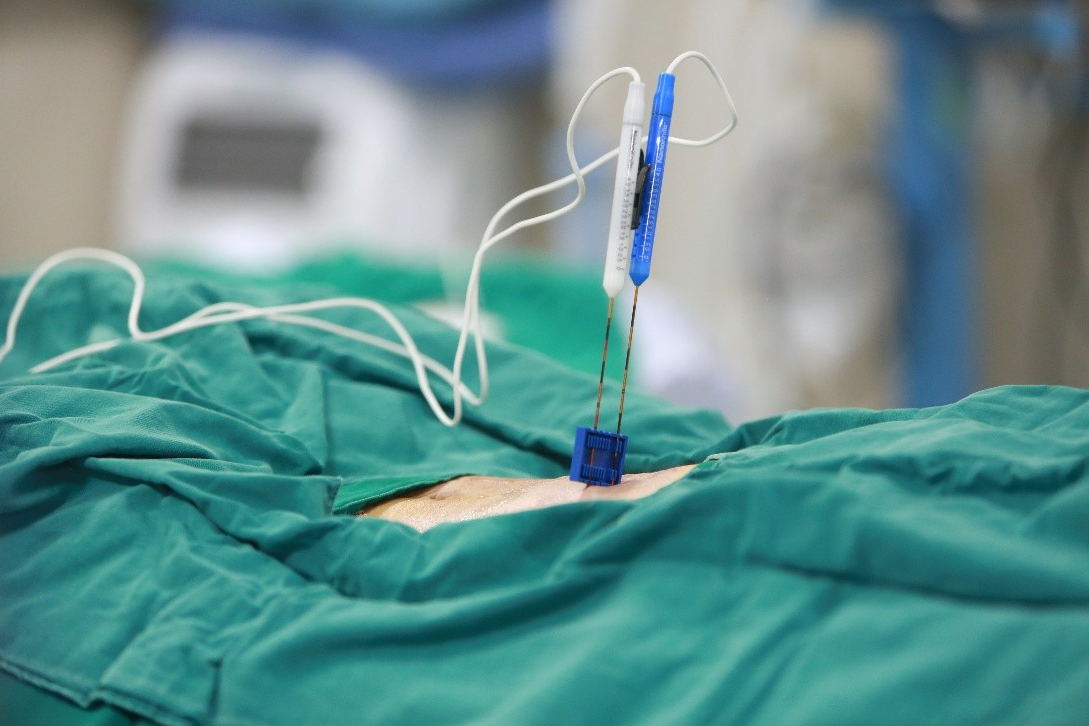
At Fuda, NanoKnife has proven particularly effective in pancreatic cancer—traditionally viewed as untreatable by ablation due to its proximity to major vessels. In Fuda’s cases, NanoKnife helped safely ablate tumors near the superior mesenteric artery, extending median survival to 22.8 months, nearly double that of traditional methods.
The Technical Matrix: Turning Despair into Possibility
Fuda has developed a comprehensive ablation matrix that includes cryoablation, NanoKnife, Gamma Knife, and seed implantation. For patients with widespread metastases like Sandi, customized treatment plans are based on tumor location, size, and blood supply:
Superficial metastases (chest wall, scalp): Cryoablation for its excellent pain-relief effect;
Lesions near central vessels (risk of pulmonary embolism): NanoKnife for precision ablation;
CNS metastases (e.g., meninges): Gamma Knife for stereotactic radiotherapy.
This tailored approach has helped Fuda achieve an 83.7% local control rate, significantly higher than the 62.4% for single-technology treatments. Meanwhile, fusion imaging (PET-CT + enhanced MRI) helps doctors accurately target active tumors and avoid overtreatment.
From Personal Miracle to Collective Hope
Sandi’s story is not unique. Among 237 advanced breast cancer patients treated with cryoablation at Fuda, 48.6% experienced tumor downgrading, and 31.2% qualified for follow-up surgery. Most importantly, average quality of life (QOL) scores rose from 38 to 86 (out of 100) post-treatment.
In an ongoing prospective study involving 386 solid tumor patients, the combination of ablation and immunotherapy resulted in a 2-year overall survival rate of 61.4%, compared to 34.7% with chemotherapy alone. Behind these numbers are countless patients like Sandi who’ve found new light in the darkness.
As oncology enters an era of precision and personalization, Fuda Cancer Hospital is building bridges of hope for patients with advanced cancer. Sandi’s story is living proof: even when facing “advanced, full-body metastases,” life can still blossom through the power of modern medicine and unwavering determination.