Cough and Chest-Back Pain—Watch Out, It Could Be Lung Cancer
Coughing and chest-back pain were Azhen’s first symptoms. The local hospital diagnosed it as a lung infection and prescribed anti-inflammatory treatment. However, after eight days of hospitalization, her condition had not improved. “Later, the hospital advised us to transfer to a cancer hospital.” Further examinations revealed an irregular nodule in the basal segment of the right lower lung lobe, possibly malignant, along with enlarged lymph nodes on both sides of the neck, raising concerns about metastasis.
Azhen was reluctant to undergo lung resection surgery, fearing the trauma and long recovery period. She and her family began seeking treatment elsewhere, hoping to find a specialized hospital that could address her condition promptly. In their search, they came across information about Guangzhou Fuda Cancer Hospital—such as its status as a national key clinical oncology hospital, its non-invasive ablation techniques, and the renowned “dual-blade hero” President Dr. Liu Lizhi—which caught their attention. After an initial online consultation, Azhen arrived at Fuda’s Department One in early September 2024.
No Surgery Needed—Freezing the Tumor to Death
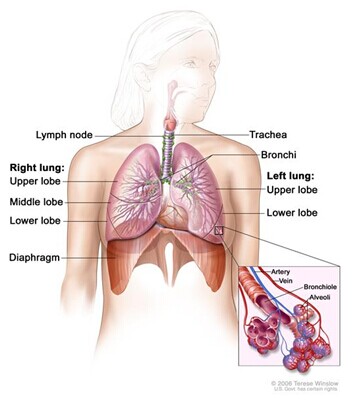
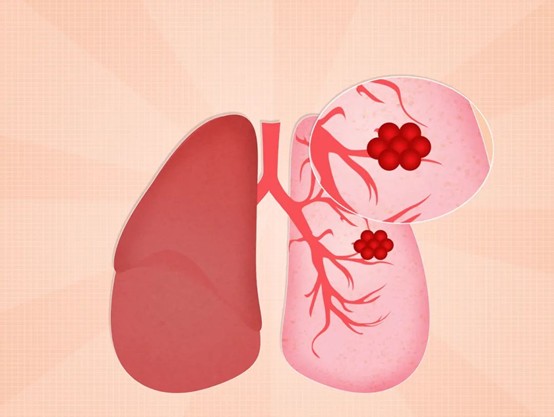
Irregular shape, high density, spiculated edges, and pleural traction—these malignant features of the lung nodule immediately raised red flags for attending physicians Dr. Shi Haiyan and Dr. Pan Zhongbao. Moreover, the presence of multiple enlarged lymph nodes in the mediastinum and right lung hilum called for heightened vigilance. Based on Azhen’s medical history and test results, and considering the presence of high-risk malignant nodules in both the upper and lower lobes of the right lung, the medical team decided on a preliminary treatment plan: percutaneous lung nodule biopsy and cryoablation, along with a biopsy of the right cervical lymph nodes.
The percutaneous biopsy helps confirm the nature of both the lung nodules and the cervical lymph nodes, while cryoablation, guided by CT imaging, involves inserting a fine probe directly into the tumor. The cancer cells are then "frozen to death" using extremely low temperatures, followed by a rewarming phase. This method effectively destroys the lesion while sparing surrounding tissues and preserving lung function. Compared to traditional surgery, cryoablation causes less pain and allows for quicker recovery. It can also be combined with other systemic treatments such as chemotherapy and targeted immunotherapy, enhancing tumor necrosis and apoptosis, and potentially extending patient survival.
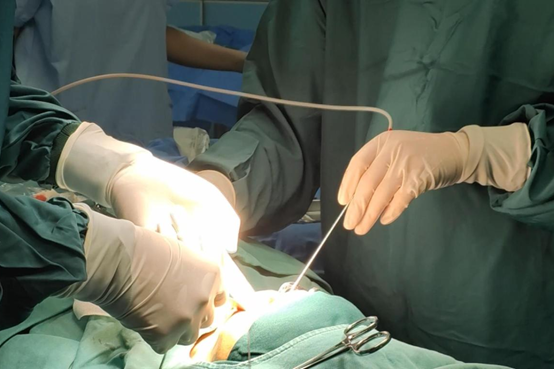
“I didn’t dare move a muscle during the procedure!” Azhen recalled. She was under local anesthesia and fully awake throughout the cryoablation, fearing any movement might shift the needle. But with President Dr. Liu Lizhi explaining the procedure in simple, reassuring terms, she gradually calmed down. “The medical staff kept chatting with me, and the whole process felt almost effortless.”
Pathological results confirmed a diagnosis of poorly differentiated adenocarcinoma in the right lung and metastatic adenocarcinoma in the right cervical lymph nodes, indicating multiple lung tumors with metastasis. Dr. Shi Haiyan explained that lung adenocarcinoma typically develops insidiously and is often not detected until it has reached the middle or late stages. In Azhen’s case, the tumor’s proximity to the pleura caused nerve irritation and pain, which fortunately prompted her to seek timely medical attention.
Comprehensive Treatment Brings More Hope
For Azhen, cryoablation alone wasn’t enough—comprehensive treatment was essential. Based on her doctors’ recommendations, she underwent genetic testing and was fortunate to find a targetable mutation, allowing her to begin oral targeted therapy. Additionally, doctors arranged multiple rounds of arterial infusion chemotherapy to control tumor progression.

“Look at my hair—it’s still thick and healthy!” Azhen exclaimed with joy. Initially, she was very worried about the side effects of chemotherapy, especially after hearing horror stories of hair loss and pallor. But arterial infusion chemotherapy completely changed her perception. “Each session takes only about 30 minutes.” During treatment, interventional doctors often chatted with her, and before she even realized it, the session would be over—leaving her with no psychological burden.
Clinically, arterial infusion chemotherapy involves delivering drugs directly into the artery feeding the tumor via a catheter. The slow, continuous infusion allows high concentrations of the drug to accumulate at the tumor site, killing cancer cells effectively without seriously harming normal tissue. Meanwhile, the drug concentration that reaches the peripheral veins is very low, greatly reducing side effects on other organs. In short, this method “reduces toxicity and increases efficacy”—a win-win.
After comprehensive treatment, Azhen’s cough and pain have significantly diminished, and the cervical lymph node metastases have visibly shrunk.
Though the Journey Was Long, She’s Grateful for Her Healing Companions
“It’s over 4,000 kilometers from Xinjiang to Guangzhou—far, tiring, and exhausting—but absolutely worth it.” Azhen likened herself to Tang Monk on his journey to the West: though filled with hardships, she overcame each challenge. Despite the long road, she found companionship and support along the way. “I must give a huge shout-out to the medical staff here!” she said, praising Fuda’s professionalism and dedication. She was especially grateful to Dr. Shi, who continued to provide timely and effective support even during her home recovery, much like a family doctor. Before her discharge, Azhen and her husband expressed their heartfelt thanks in a letter and custom-made a silk banner to present to the staff.

“We may not be rich, but our life is comfortable; our children are doing well, so we have no worries. All we need is a good mindset and scientific treatment.” Now, Azhen hopes for continued health and dreams of traveling and relaxing wherever and whenever she can.