Surgical resection is the primary treatment for most malignant tumors. But what if the tumor is in a complex or critical area—wrapped around blood vessels, invading nerves, adjacent to vital structures, or in a location too complex for surgery?
Take the so-called "king of cancers"—pancreatic cancer—as an example. Due to the pancreas’s deep and complex anatomical location, surgery is challenging. Moreover, many cases are diagnosed at a late stage, resulting in a 5-year survival rate that remains dismally low. Fewer than 20% of patients are eligible for surgery at the time of diagnosis.
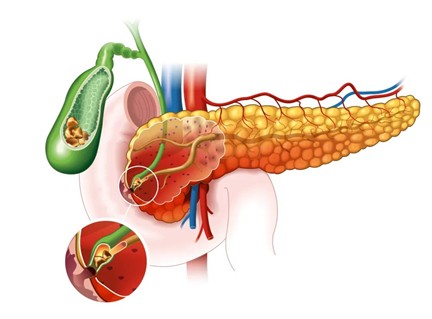
In many cases, pancreatic tumors encase vital blood vessels such as the superior mesenteric artery and vein, or the celiac artery, making surgery highly risky and technically difficult. While radiotherapy or chemotherapy are often used, pancreatic cancer is not very responsive to either, and patient prognosis remains poor.
Traditional thermal ablation techniques—like radiofrequency ablation, microwave ablation, and cryoablation—damage both tumor and nearby tissue indiscriminately. Because they rely on temperature-based destruction, these methods often harm surrounding structures, potentially causing severe complications.
This is where a new, non-thermal, selective, and tissue-sparing technology comes in—NanoKnife Ablation.
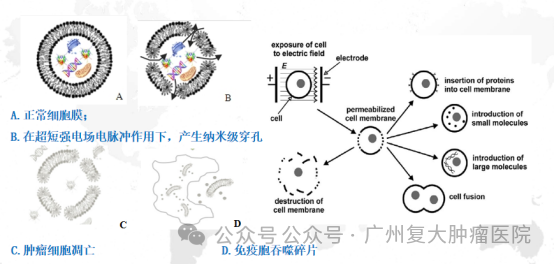
The scientific term for NanoKnife is Irreversible Electroporation (IRE). It uses high-voltage, microsecond-length electric pulses to create permanent nanopores in tumor cell membranes, triggering cell death while preserving critical structures. Unlike traditional surgery, NanoKnife minimizes risks such as bleeding and allows physicians to "have their cake and eat it too."

NanoKnife technology uses 3000-volt short electrical pulses to perforate the tumor cell membrane. Electro-pulse patterns are clearly visible on ECG during treatment. It is highly effective for pancreatic cancer and hilar liver cancer.
Recent studies show promising results:
•Martin et al. reported over 200 pancreatic cancer patients treated with NanoKnife with overall survival (OS) exceeding 2 years.
•A multicenter international study showed an OS of 30 months.
•An Asian multicenter trial combining S1 chemotherapy with IRE showed an OS of 28.7 months.
Due to such encouraging outcomes, China’s National Health Commission has included irreversible electroporation in the 2022 Pancreatic Cancer Diagnosis and Treatment Guidelines. Several international consensus statements and clinical guidelines also recommend its use.
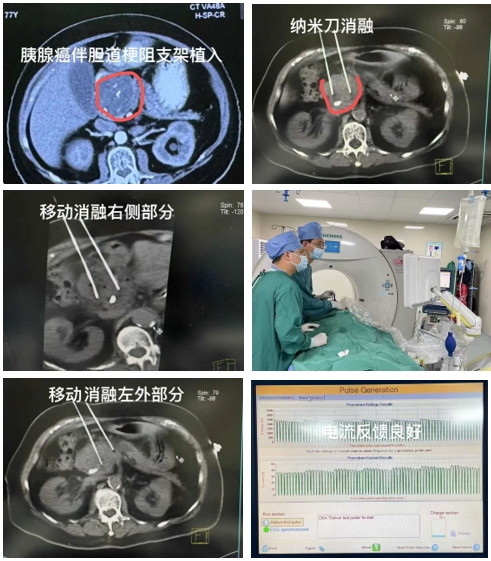

A pancreatic cancer patient from the Philippines, who could not undergo surgery and had a biliary stent placed locally, traveled to China specifically for NanoKnife treatment. The patient had a 5.3 cm tumor in the pancreatic head—complex and difficult to treat. Under ultrasound and CT guidance, we used a mobile ablation approach to successfully complete NanoKnife ablation.
NanoKnife also shows significant advantages for tumors near delicate areas such as:
•Liver hilum
•Bile ducts
•Gallbladder
•Ureters
Tumors in the liver hilum are nearly impossible to remove surgically, and thermal ablation is risky due to potential damage to essential hepatic structures. Why can NanoKnife preserve bile ducts, pancreatic ducts, blood vessels, and even the intestines, ensuring faster functional recovery post-treatment?
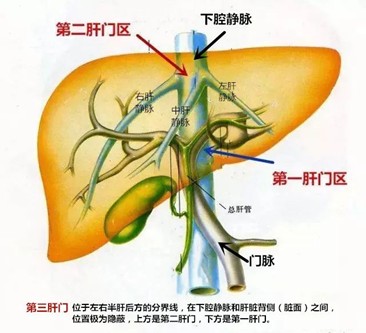
Because NanoKnife doesn’t rely on heat. Instead, it uses high-frequency electrical pulses to induce cell death without destroying anatomical structures, avoiding the risks of incomplete ablation or thermal injury.
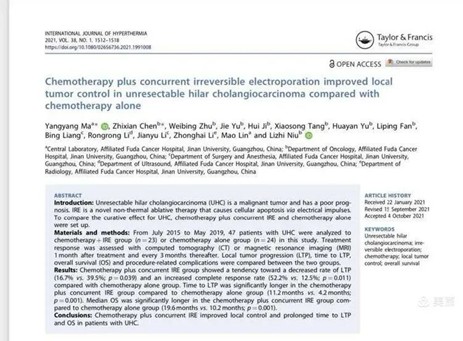
Professor Anna from the University of Rome led a literature review and meta-analysis on NanoKnife for hilar cholangiocarcinoma. After screening 627 articles, six studies were selected for detailed quantitative analysis.

Key findings:
•NanoKnife + chemotherapy: Average survival time of 25 months.
•100% bile duct recanalization rate, indicating significantly improved quality of life.
Even with certain limitations, the survival benefit for patients with unresectable hilar cholangiocarcinoma was substantial.
One of the cited studies came from our hospital—the first in the world to propose a synchronous NanoKnife + chemotherapy protocol. This method enhances the tumor-killing effects of NanoKnife while leveraging its electrochemical and immune-modulating benefits. This combined approach offers synergistic efficacy, especially for cancers that are traditionally hard to ablate—similar in concept to chemoradiotherapy, but safer and more effective.
For prostate tumors, traditional ablation methods can damage nerves and result in sexual dysfunction. NanoKnife, by preserving nerves and ducts, offers an irreplaceable option for these patients.
NanoKnife ablation offers a new and effective local treatment for malignant tumors in anatomically challenging and surgically inaccessible regions.