A pancreatic tumor has spread to the liver, making surgery impossible. Is there still hope for treatment?
Hesha (pseudonym), a patient from Egypt, was diagnosed with pancreatic cancer and liver metastasis. Unfortunately, his tumor was detected during a routine health check when it was already in the advanced stage, and surgery was not an option. The local hospital informed him that chemotherapy was the only treatment available. However, chemotherapy caused significant suffering, and within just three months, he lost over 30 pounds.
Hesha sought medical care in several countries but was always presented with chemotherapy as the only treatment. Reluctant to endure the pain of chemotherapy any longer, he eventually learned about Fuda Cancer Hospital's cryoablation therapy through a Chinese friend. This alternative treatment sparked hope in him, and he decided to travel to China in search of a solution.
In mid-April 2024, Hesha traveled thousands of miles to Guangzhou, China, and arrived at the Medical Department II of Fuda Cancer Hospital. At the time, he was in severe pain, and imaging results revealed a mass measuring approximately 6.4×6.4×4.0 cm at the body and tail of his pancreas, which was adhered to adjacent tissues. Multiple lymph node enlargements were observed in the bilateral lung hila, mediastinum, bilateral axilla, hepatic hilum, retroperitoneum, and mesenteric area. These symptoms led to significant weakness, loss of appetite, and a sense of hopelessness.

Medical Examination by Dr. Wang Feng
After thorough discussion among specialists, the doctors determined that, due to the advanced stage of the tumor and lack of surgical options, palliative care was the primary approach. After consulting with Hesha and his family, the medical team decided on a treatment plan that included pancreatic tumor cryoablation combined with iodine-125 particle implantation. This treatment aimed to locally inactivate the tumor, followed by interventional chemotherapy to control tumor growth.
By early November 2024, Hesha had returned for a follow-up appointment. Imaging revealed that his pancreatic tumor had shrunk, and lymph nodes in several areas had also decreased in size. His condition had stabilized, and most importantly, his pain had been alleviated. Hesha reported feeling much better and was hopeful for further improvement in the coming treatments.
Why is Pancreatic Cancer Often Diagnosed at an Advanced Stage?
Hesha's cancer was detected during a routine check-up, but he had no prior symptoms. By the time the tumor was discovered, it was already too late for surgery. Pancreatic cancer originates in the ductal cells of the pancreas. The pancreas is located deep within the body, behind the stomach, omentum, and colon, which makes early tumors difficult to detect during routine examinations.

Moreover, the pancreas has limited nerve distribution, so early tumors do not cause noticeable pain. Symptoms such as vague upper abdominal discomfort, nausea, bloating, indigestion, and fatigue are easily confused with gastrointestinal or liver diseases. As a result, many patients do not receive a diagnosis until they exhibit more serious symptoms such as jaundice, ascites, mass formation, or back pain, which often indicates the disease is already in an advanced stage.
In terms of treatment, locally advanced and metastatic pancreatic cancer cannot be cured. Even with significant advances in surgical and radiation techniques, not all patients benefit from these treatments. Traditional therapies do not resolve the fundamental issue of how to improve the quality of life and extend the survival of patients with inoperable pancreatic cancer.
Hesha's treatment involved the use of iodine-125 particle implantation and cryoablation, both of which are currently widely used new technologies. Iodine-125 particle implantation, also known as interstitial brachytherapy, involves placing sealed radioactive sources directly into the tumor under imaging guidance, allowing them to continuously release radiation to kill tumor cells. This method has been shown to be safe and effective for advanced pancreatic cancer, suppressing tumor growth and significantly relieving pain. Additionally, it can enhance the sensitivity of the tumor to other treatments, such as chemotherapy and ablation.

Cryoablation, which uses extremely low temperatures to destroy tumor cells, is one of the earliest methods tried for tumor treatment. This technique involves inserting a special cryoprobe into the tumor tissue under imaging guidance, rapidly lowering the temperature of the tumor, causing cancer cells to die from extreme cold. When combined with iodine-125 particle implantation, cryoablation provides a higher survival rate and longer median overall survival (OS) compared to cryotherapy alone. This combined approach is a promising option for patients with locally advanced or inoperable pancreatic cancer, helping to avoid the adverse effects of chemotherapy or radiation.

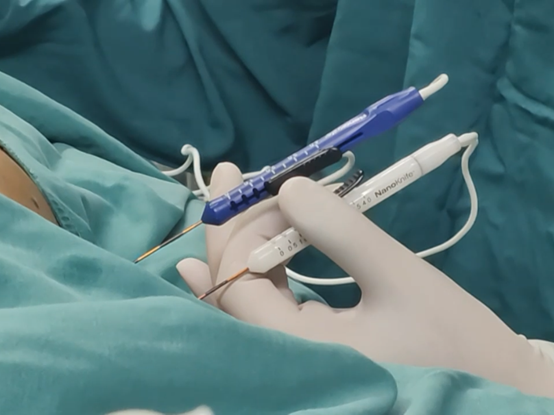
In addition to these therapies, Fuda Cancer Hospital also offers Nanoknife treatment for inoperable pancreatic cancer. Known as irreversible electroporation (IRE), this new non-physical ablation technique selectively targets and destroys tumor tissue while preserving nearby vital structures. When combined with other treatments such as chemotherapy, targeted therapy, and immunotherapy, Nanoknife can significantly reduce clinical symptoms and extend survival. The hospital has performed over 1,000 Nanoknife procedures, gaining substantial clinical experience.
Hesha's case demonstrates the potential of combining advanced therapies like iodine-125 particle implantation, cryoablation, and Nanoknife to treat advanced pancreatic cancer. These innovative approaches offer hope for patients who were previously limited to palliative care or chemotherapy alone. Fuda Cancer Hospital continues to be at the forefront of providing cutting-edge treatment options for cancer patients worldwide.