Rhabdomyosarcoma (RMS) is a malignant soft tissue tumor originating from immature skeletal muscle cells. It primarily affects children and adolescents but can also occur in adults. This tumor can develop in various parts of the body, including the head and neck region, urogenital system, extremities, and thoracoabdominal areas. Below are some key points:
Classification
Rhabdomyosarcoma is classified into several subtypes based on histological and molecular characteristics:
- Embryonal RMS:
- The most common subtype, accounting for the majority of cases.
- Frequently occurs in children, typically in the head and neck region (e.g., around the orbit), urogenital system, or trunk.
- Alveolar RMS:
- More common in adolescents and young adults.
- Usually affects the extremities, trunk, or chest wall and is associated with higher malignancy.
- Pleomorphic RMS:
- Rare and primarily seen in adults.
- Highly malignant with a poorer prognosis.
- Spindle Cell/Sclerosing RMS:
- A rare subtype with distinct pathological features.
Causes and Risk Factors
While the exact causes are not fully understood, the following factors may increase the risk:
- Genetic Factors:
- Conditions such as Li-Fraumeni syndrome and neurofibromatosis type 1 (NF1) are associated with higher risk.
- Environmental Factors:
- Potential links to maternal exposure to carcinogens during pregnancy.
Symptoms
Symptoms vary depending on the tumor's location:
- Head and Neck: Lump, proptosis (bulging eyes), nasal congestion, or nosebleeds.
- Urogenital System: Hematuria (blood in urine), difficulty urinating, or abnormal vaginal discharge.
- Extremities: Lump or localized pain.
- Thoracoabdominal Region: Abdominal swelling or pain.
Diagnosis
Diagnosis involves a combination of clinical assessment, imaging, and pathological evaluation:
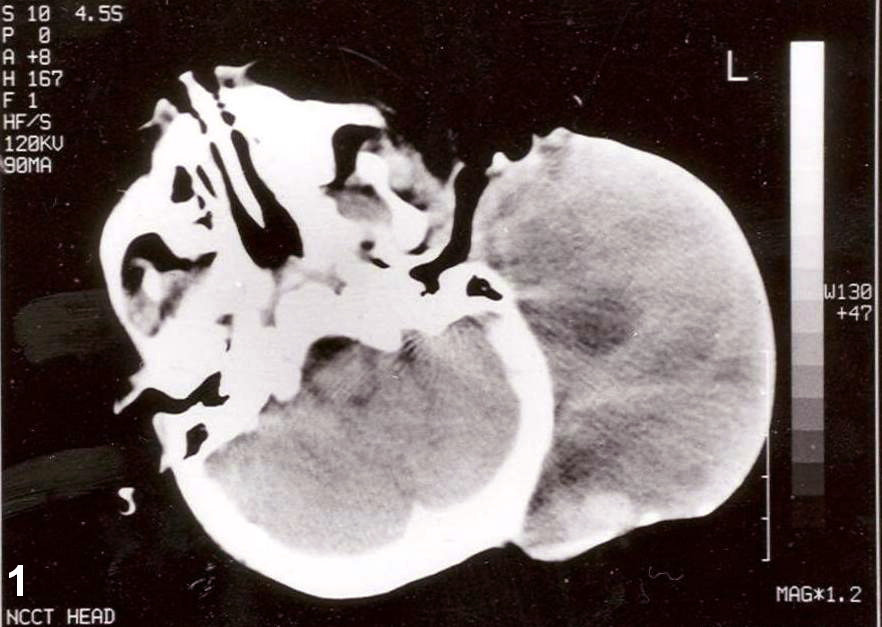
1. Imaging Studies:
- CT, MRI, ultrasound, or PET-CT to assess tumor location, size, and spread.
2. Pathological Examination:
- Biopsy to confirm diagnosis, supported by immunohistochemistry (e.g., markers like myosin and desmin) to determine tumor type.
3. Molecular Testing:
- Specific chromosomal translocations (e.g., PAX3-FOXO1 or PAX7-FOXO1) in certain subtypes (like alveolar RMS).
Treatment
Treatment typically involves a multidisciplinary approach, including:
1. Surgery:
- Aiming for complete tumor removal.
2. Chemotherapy:
- Multi-agent regimens such as VAC (vincristine, actinomycin D, and cyclophosphamide).
3. Radiotherapy:
- For unresectable tumors or residual disease post-surgery.
4. Targeted and Immunotherapy:
- Potential applications for advanced or recurrent cases.
5. Minimally Invasive Interventional Therapies
These approaches are suitable for patients with inoperable or advanced rhabdomyosarcoma, aiding in tumor control or serving as adjunctive treatments.
Radiofrequency Ablation (RFA) or Microwave Ablation (MWA):
Destroys tumor tissue through high-frequency electrical currents or microwave heating.
Often used for localized recurrences or unresectable tumors.
Transarterial Chemoembolization (TACE):
Delivers chemotherapeutic drugs and embolic agents directly into the tumor's arterial supply, blocking blood flow and killing cancer cells.
Particularly effective for deep-seated or surgically inaccessible tumors.
Cryoablation:
Uses low-temperature techniques to freeze tumor tissues, suitable for heat-resistant or tumors adjacent to critical structures.
Prognosis
The prognosis of rhabdomyosarcoma depends on the following factors:
- Tumor Type:
- Embryonal RMS has a better prognosis, while alveolar RMS is associated with poorer outcomes.
- Location:
- Superficial tumors are more treatable, whereas deep-seated or tumors near vital organs are more challenging.
- Stage:
- Early-stage cases have higher cure rates, while late-stage disease carries a worse prognosis.
- Patient Age:
- Younger patients generally respond better to treatment.