Cervical cancer is a malignant neoplasm arising from cells originating in the cervix uteri. One of the most common symptoms of cervical cancer is abnormal vaginal bleeding, but in some cases there may be no obvious symptoms until the cancer has progressed to an advanced stage.
Treatment usually consists of surgery (including local excision) in early stages, and chemotherapy and/or radiotherapy in more advanced stages of the disease.
Cancer screening using the Pap smear can identify precancerous and potentially precancerous changes in cervical cells and tissue. Treatment of high-grade changes can prevent the development of cancer in many victims. In developed countries, the widespread use of cervical screening programs has dramatically reduced the incidence of invasive cervical cancer.
Human papillomavirus (HPV) infection appears to be a necessary factor in the development of almost all cases (90+%) of cervical cancer. HPV vaccines effective against the two strains of this large family of viruses that currently cause approximately 70% of cases of cervical cancer have been licensed in the U.S, Canada, Australia, and the EU.Since the vaccines only cover some of the cancer-causing ("high-risk") types of HPV, women should seek regular Pap smear screening, even after vaccination.
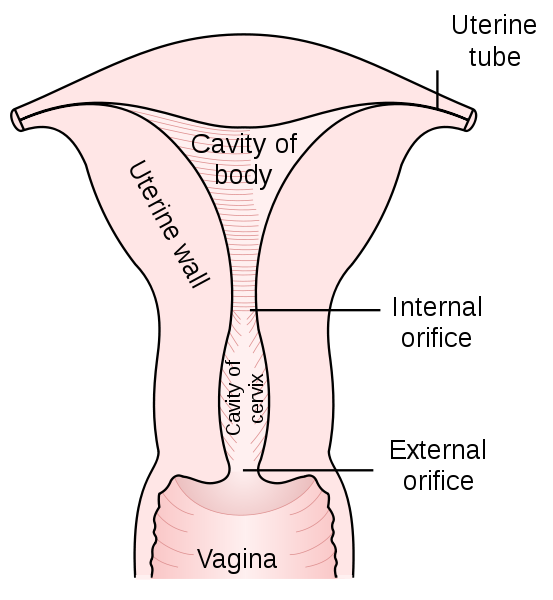
The cervix is the narrow portion of the uterus where it joins with the top of the vagina. Most cervical cancers are squamous cell carcinomas, arising in the squamous (flattened) epithelial cells that line the cervix. Adenocarcinoma, arising in glandular epithelial cells is the second most common type. Very rarely, cancer can arise in other types of cells in the cervix.
Signs and symptoms
The early stages of cervical cancer may be completely asymptomatic.[1][2] Vaginal bleeding, contact bleeding, or (rarely) a vaginal mass may indicate the presence of malignancy. Also, moderate pain during sexual intercourse and vaginal discharge are symptoms of cervical cancer. In advanced disease, metastases may be present in the abdomen, lungs or elsewhere.
Symptoms of advanced cervical cancer may include: loss of appetite, weight loss, fatigue, pelvic pain, back pain, leg pain, swollen legs, heavy bleeding from the vagina, bone fractures, and/or (rarely) leakage of urine or faeces from the vagina.
Causes
Infection with some types of human papilloma virus (HPV) is the greatest risk factor for cervical cancer, followed by smoking. Other risk factors include human immunodeficiency virus.[8] Not all of the causes of cervical cancer are known, however, and several other contributing factors have been implicated.
Human papillomavirus
Human papillomavirus type 16 and 18 are the cause of 70% of cervical cancer globally while 31 and 45 are the cause of another 10%.
Women who have many sexual partners (or who have sex with men who have had many other partners) have a greater risk.
Of the 150-200 types of HPV known,[14][15] 15 are classified as high-risk types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82), 3 as probable high-risk (26, 53, and 66), and 12 as low-risk (6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81, and CP6108).
Genital warts, which are a form of benign tumor of epithelial cells, are also caused by various strains of HPV. However, these serotypes are usually not related to cervical cancer. It is common to have multiple strains at the same time, including those that can cause cervical cancer along with those that cause warts. The medically accepted paradigm, officially endorsed by the American Cancer Society and other organizations, is that a patient must have been infected with HPV to develop cervical cancer, and is hence viewed as asexually transmitted disease (although many dispute that, technically, it is the causative agent, not the cancer, that is a sexually transmitted disease), but most women infected with high risk HPV will not develop cervical cancer.[17] Use of condoms reduces, but does not always prevent transmission. Likewise, HPV can be transmitted by skin-to-skin-contact with infected areas. In males, there is no commercially available test for HPV, although HPV is thought to grow preferentially in the epithelium of the glans penis, and cleaning of this area may be preventative.
Smoking
Smoking has also been linked to the development of cervical cancer.There are a few different ways that smoking can increase the risk of cervical cancer in women which can be by direct and indirect methods of inducing cervical cancer. A direct way of contracting this cancer is a female smoker has a higher chance of CIN3 occurring which has the potential of forming cervical cancer.When CIN3 lesions lead to cancer, most of them have the assistance of the HPV virus, but that is not always the case which is why it can be considered a direct link to cervical cancer. An indirect means of developing this cancer by smoking is that it can lead to human papillomavirus which can result in cervical cancer.Heavy smoking and long term smoking seem to have more of a risk of getting the CIN3 lesions than lighter smoking or not smoking at all.Although smoking has been linked to cervical cancer, it aids in the development of HPV which is the leading cause of this type of cancer.Also, not only does it aid in the development of HPV, but if the woman is already HPV-positive she is at an even greater likelihood of contracting cervical cancer.
Diagnosis
Biopsy
While the pap smear is an effective screening test, confirmation of the diagnosis of cervical cancer or pre-cancer requires a biopsy of the cervix. This is often done through colposcopy, a magnified visual inspection of the cervix aided by using a diluteacetic acid (e.g. vinegar) solution to highlight abnormal cells on the surface of the cervix.[1] Medical devices used for biopsy of the cervix include punch forceps, SpiraBrush CX, SoftBiopsy or Soft-ECC.
Colposcopic impression, the estimate of disease severity based on the visual inspection, forms part of the diagnosis.
Further diagnostic and treatment procedures are loop electrical excision procedure (LEEP) and conization, in which the inner lining of the cervix is removed to be examined pathologically. These are carried out if the biopsy confirms severe cervical intraepithelial neoplasia.
Precancerous lesions
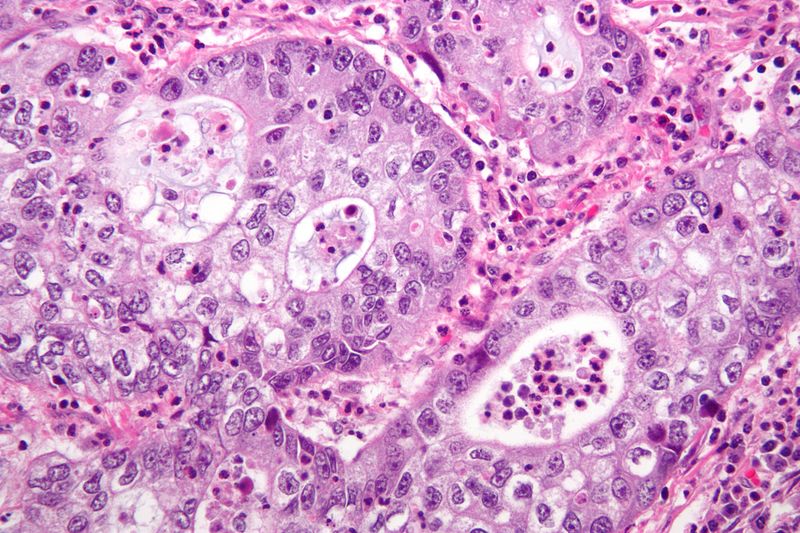
Cervical intraepithelial neoplasia, the potential precursor to cervical cancer, is often diagnosed on examination of cervical biopsies by a pathologist. For premalignant dysplastic changes, the CIN (cervical intraepithelial neoplasia) grading is used.
The naming and histologic classification of cervical carcinoma percursor lesions has changed many times over the 20th century. The World Health Organization classification system was descriptive of the lesions, naming them mild, moderate or severe dysplasia or carcinoma in situ (CIS). The term, Cervical Intraepithelial Neoplasia (CIN) was developed to place emphasis on the spectrum of abnormality in these lesions, and to help standardise treatment.[24] It classifies mild dysplasia as CIN1, moderate dysplasia as CIN2, and severe dysplasia and CIS as CIN3. More recently, CIN2 and CIN3 have been combined into CIN2/3. These results are what a pathologist might report from a biopsy.
These should not be confused with the Bethesda System terms for Pap smear (cytopathology) results. Among the Bethesda results: Low-grade Squamous Intraepithelial Lesion (LSIL) and High-grade Squamous Intraepithelial Lesion (HSIL). An LSIL Pap may correspond to CIN1, and HSIL may correspond to CIN2 and CIN3,[24] however they are results of different tests, and the Pap smear results need not match the histologic findings.
Cancer subtypes
Histologic subtypes of invasive cervical carcinoma include the following:[25][26] Though squamous cell carcinoma is the cervical cancer with the most incidence, the incidence of adenocarcinoma of the cervix has been increasing in recent decades.
squamous cell carcinoma (about 80-85%[citation needed])
adenocarcinoma (about 15% of cervical cancers in the UK)
adenosquamous carcinoma
small cell carcinoma
neuroendocrine tumour
glassy cell carcinoma
villoglandular adenocarcinoma
Non-carcinoma malignancies which can rarely occur in the cervix include
melanoma
lymphoma
Note that the FIGO stage does not incorporate lymph node involvement in contrast to the TNM staging for most other cancers.
For cases treated surgically, information obtained from the pathologist can be used in assigning a separate pathologic stage but is not to replace the original clinical stage.
Staging
Main article: Cervical cancer staging
Cervical cancer is staged by the International Federation of Gynecology and Obstetrics (FIGO) staging system, which is based on clinical examination, rather than surgical findings. It allows only the following diagnostic tests to be used in determining the stage: palpation, inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, intravenous urography, and X-ray examination of the lungs and skeleton, and cervical conization.
Prevention
Screening
The widespread introduction of cervical screening by the Papanicolaou test, or Pap smear for cervical cancer has been credited with dramatically reducing the incidence and mortality of cervical cancer in developed countries. Pap smear screening every 3–5 years with appropriate follow-up can reduce cervical cancer incidence by up to 80%.Abnormal results may suggest the presence of pre cancerous changes allowing examination and possible preventive treatment. If precancerous disease or cervical cancer is detected early, it can be monitored or treated relatively noninvasively, with little impairment of fertility.
Cervical cancer screening is typically recommended starting at age 21.Recommendations for how often a Pap smear should be done vary from once a year to once every five years, in the absence of abnormal results.[Guidelines vary on how long to continue screening, but well screened women who have not had abnormal smears can stop screening about age 60 to 70.
Liquid-based cytology is another potential screening method.[33][34] Although it was probably intended to improve on the accuracy of the Pap test, its main advantage has been to reduce the number of inadequate smears from around 9% to around 1%.[35] This reduces the need to recall women for a further smear. The United States Preventive Services Task Force supports screening every 5 years in those who are between 30 and 65 years when cytology is used in combination with HPV testing.
Vaccination
There are two HPV vaccines (Gardasil and Cervarix) which reduce the risk of cancerous or precancerous changes of the cervix and perineum by about 93%.
HPV vaccines are typically given to women age 9 to 26 as the vaccine is only effective if given before infection occurs. The vaccines have been shown to be effective for at least 4[6] to 6[38] years, and it is believed they will be effective for longer;[39] however, the duration of effectiveness and whether a booster will be needed is unknown. The high cost of this vaccine has been a cause for concern. Several countries have considered (or are considering) programs to fund HPV vaccination.
Condoms
Condoms are thought to offer some protection against cervical cancer.Evidence on whether condoms protect against HPV infection is mixed, but they may protect against genital warts and the precursors to cervical cancer. They also provide protection against other STDs, such as HIV and Chlamydia, which are associated with greater risks of developing cervical cancer.
Condoms may also be useful in treating potentially precancerous changes in the cervix. Exposure to semen appears to increase the risk of precancerous changes (CIN 3), and use of condoms helps to cause these changes to regress and helps clear HPV.[41] One study suggests thatprostaglandin in semen may fuel the growth of cervical and uterine tumours and that affected women may benefit from the use of condoms.
Nutrition
Vitamin A is associated with a lower risk[44] as is vitamin B12, vitamin C, vitamin E, and beta-carotene.