Meigs syndrome refers to benign solid ovarian tumors such as fibroma, fibroepithelioma, theca cell tumor, granulosa cell tumor, sclerosing stromal tumor, etc., combined with signs such as abdominal effusion and pleural effusion. In primary ovarian tumors A group of clinical syndromes in which pleural and abdominal effusions disappear after resection. The syndrome was first reported by Joe Vincent Meigs in 1937.
Cases of other pathological types of benign pelvic tumors combined with pleural effusion and ascites have also been continuously revealed, including benign ovarian teratoma, mucinous cystadenoma, fallopian tube papilloma, and ovarian malignant tumors such as Krukenberg tumor, and non-ovarian tumors such as renal pelvic transitional cell tumors are also combined with pleural effusion and other signs to varying degrees. Therefore, some experts call the various non-ovarian benign solid tumors pseudo-Meigs syndrome. Pseudo-Meigs syndrome is rare in clinical practice, with a low incidence rate and is easily misdiagnosed.

▲Liu Shupeng, deputy director of the Fifth Medical Department of Guangzhou Fuda Cancer Hospital, shared his medical records
Recently, the Fifth Department of Medical Care of Guangzhou Fuda Cancer Hospital successively admitted two patients with pseudo-Meigs syndrome caused by colon cancer, which occurred in colon cancer and later metastasized to the ovary, causing a large amount of ascites and pleural effusion. After resection, long-term survival can be achieved. There are currently very few reports in the literature as only 11 cases of colorectal cancer found in foreign countries, and there are no relevant reports in China.
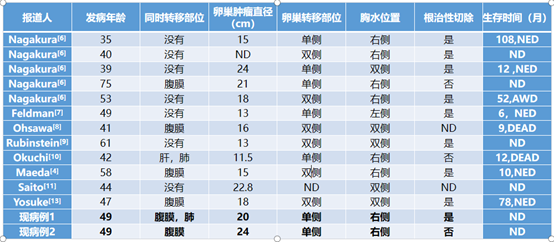
▲Case reports of pseudo-Meigs syndrome caused by ovarian metastasis from colorectal cancer
Case One
Patient Ms. C diagnosed with advanced stage of colon malignant tumor, accompanied by a huge pelvic mass, which caused abdominal distension, intestinal obstruction, and symptoms such as pleural effusion and ascites. Based on the past medical history and the actual situation, the doctor raised the following questions: ① What is the cause of intestinal obstruction? Is it caused by colon cancer or oppression by ovarian tumors? ②What is the relationship between colon cancer and giant ovarian tumors? ③Does pleural effusion mean there is a transfer?
With these questions, the doctor conducted a comprehensive examination of the patient and found several favorable evidences: ① The ovarian tumor was huge, but it did not surround the intestines and large blood vessels and was relatively independent and complete; ② The intestinal obstruction was caused by the huge squeezing of the ovarian tumor; ③ There was pleural effusion and ascites, but no lesions were found, and the pleural effusion did not decrease significantly during chemotherapy.
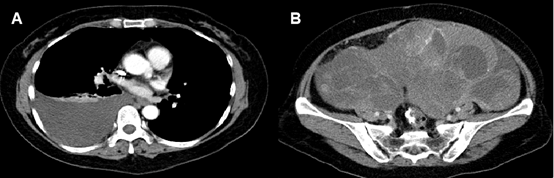
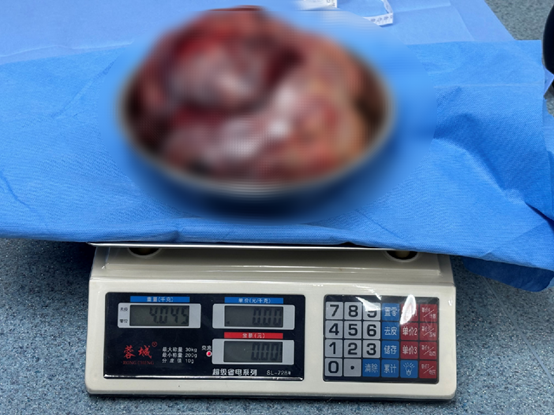
These findings made the patient's surgery possible. After a series of preparations, our hospital's experts removed a huge mass measured 24×24×20 cm and 3.6kg. Five days after the operation, the patient's pleural effusion and ascites also disappeared. The lesions suggested (abdomen and pelvis) metastatic adenocarcinoma, which was considered to be metastasis of intestinal cancer.
Case Two
Ms. Z, the patient, suffered from lower abdominal pain, accompanied by blood in the stool, constipation, abnormal uterine bleeding during menstruation, dizziness, chest tightness and shortness of breath. In early 2023, she was diagnosed with intestinal cancer accompanied by tumors in the right adnexal area and abdominal cavity, retroperitoneal lymph nodes and peritoneum. She underwent surgery and chemotherapy at a local hospital. A review at the end of 2023 found that the pelvic tumor was significantly larger than before, compressing the intestines and causing intestinal obstruction, and there was no significant reduction after drainage of pleural and abdominal effusions.
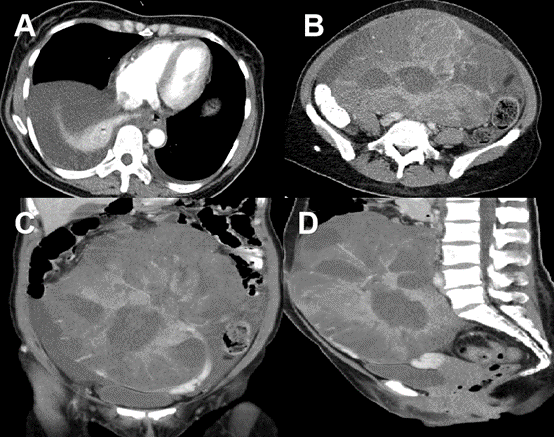
In the end, experts from Fuda also performed surgery to completely remove the huge mass of 24×24×20 cm. Three days after the operation, the patient’s pleural effusion also disappeared. The lesions were also consistent with abdominal and pelvic metastatic adenocarcinoma, and were considered to be gastroenteral cancer metastasis.

The treatment currently of pseudo-Meigs syndrome is surgical removal of giant ovarian tumors. After surgical resection, the pleural and abdominal effusions in most patients disappear, and the clinical prognosis is good, and the patients can survive for a long time. Of course, some patients with more serious underlying diseases are not suitable for surgical resection, and symptomatic drainage of pleural and abdominal effusions can also achieve the effect of alleviating clinical symptoms.
In the case with intestinal cancer + huge ovarian metastasis + pleural effusion + ascites, etc., most people would think the patient is in the late stage, with tumor recurrence or multiple metastases, and that further treatment is not possible. The two patients therefore underwent palliative treatments such as chemotherapy or targeted immunotherapy, but the results were unsatisfactory.
However, Guangzhou Fuda Cancer Hospital combined clinical practice and theory. After a clear diagnosis of pseudo-Meigs syndrome and surgical removal of ovarian tumors, those two patients’ pleural and abdominal effusions completely disappeared and there was no obvious recurrence. Currently, they continue to receive postoperative adjuvant chemotherapy treatment to prevent disease progression.