After oral mucosal injury, local microorganisms multiply extensively, causing progressive worsening of the wound, which not only severely affects the quality of life of tumor patients but can also lead to treatment interruption, affecting the efficacy of the primary disease treatment. So, what should be done when oral mucositis occurs during anti-tumor treatment? Recently, Li Yanhong, the head nurse of the first medical department at Fuda Cancer Hospital shared related content.

The oral cavity hosts the second largest and most diverse microbial community after the intestines. These microbial communities have stable and diverse characteristics, which can prevent the colonization of exogenous pathogens and the overgrowth of endogenous pathogens, maintaining normal physiological processes and mucosal immune responses of the host. Once external factors lead to changes in the composition of symbiotic flora, dysbiosis occurs, which may cause an imbalance in host immune responses and increase the risk of disease for the host.
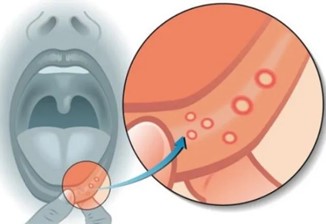
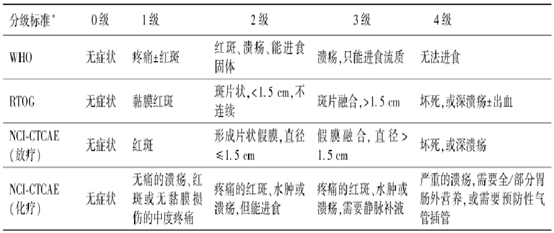
Oral mucositis (OM) refers to inflammatory and/or ulcerative lesions of the oral mucosal epithelium. For patients with malignant tumors, radiotherapy, chemotherapy, targeted therapy, or immunotherapy are the main causes of oral mucositis. There are significant differences in the incidence of OM among patients with different types of tumors and those receiving different treatments.
![]()
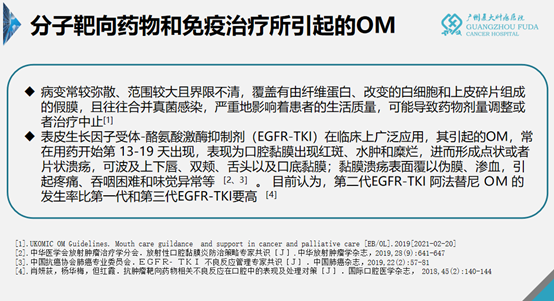
The incidence of oral mucositis in patients treated with targeted drugs can be as high as 30-50%. These lesions are often diffuse, extensive, and poorly demarcated, covered with pseudomembrane composed of fibrin, altered leukocytes, and epithelial debris, and often accompanied by fungal infections.
As a new treatment for lung cancer, oral mucositis caused by epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKI) usually occurs between the 13th and 19th day after medication. It often manifests as erythema, edema, and erosion of the oral mucosa, progressing to punctate or patchy ulcers that can affect the upper and lower lips, cheeks, tongue, and floor of the mouth. The mucosal ulcer surface is covered with pseudomembrane and exudate, causing pain, difficulty swallowing, and taste disturbances.
This not only causes severe oral pain, affecting the patient's eating, speaking, and resting, but also may reduce the patient's tolerance and compliance with anti-tumor treatment, delaying or even stopping treatment, and reducing the quality of life and anti-tumor efficacy.
Currently, Western medicine prevention mainly draws on the prevention and treatment of radiotherapy and chemotherapy-related oral mucositis, and there is still a lack of high-quality clinical trial support. Inhibitor-associated stomatitis (mIAS) is mostly discussed in this context. These measures are mainly summarized as oral care, supportive treatment, anti-inflammatory treatment, and other treatments. When symptoms are severe (such as severe pain, affecting oral intake), dose reduction or discontinuation of EGFR-TKI-related drugs should be considered.
Common oral care measures include keeping the patient's mouth moist and clean; avoiding damage to the oral mucosa by using a soft-bristled toothbrush; avoiding the use of tobacco, alcohol, and irritating foods such as spicy and acidic foods; and using mild mouthwashes such as saline or sodium bicarbonate solutions to help maintain oral hygiene and improve patient comfort. Compound chlorhexidine (Hibitane) is also often used as an oral disinfectant; it has a minimal impact on the oral microbiome and can be used to prevent oral infections.
In addition, several domestic scholars have observed that the use of moist burn ointment (MEBO) in the treatment of 30 cases of radiation-induced oral mucositis effectively promotes oral mucosal repair and shortens the treatment time. MEBO is a traditional Chinese medicine single-ointment preparation containing Coptis, Scutellaria, and Phellodendron, which have the effects of clearing heat and dampness, purging fire and detoxifying; and Poppy shell and Earthworm, which have the effects of promoting blood circulation, relieving pain, promoting muscle growth, and astringing. It can effectively prevent and treat the blockage of meridians and stagnation of qi and blood in the wound, thereby promoting wound healing. Modern medical research confirms that the active ingredients in MEBO can form a protective film on the wound surface, controlling and isolating bacterial invasion, providing a favorable environment for wound recovery.
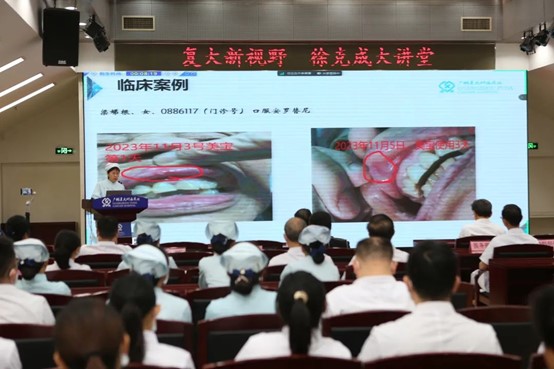
To evaluate the efficacy and safety of MEBO in the treatment of tyrosine kinase inhibitor-associated oral mucositis, reduce the degree of mucosal damage during the window period of EGFR-TKI-associated oral mucositis, shorten the treatment and care time for oral mucositis, and allow for the continued clinical use of EGFR-TKI or its continued use after oral mucositis downgrade, Li Yanhong and her team conducted a grouped study based on pathological diagnosis. The study included patients with gene detection indicating EGFR-sensitive mutations, inoperable or advanced non-small cell lung cancer (NSCLC), recommended by a multidisciplinary physician consultation to use EGFR-TKI, who started or had been receiving EGFR-TKI treatment for more than one week, and had grade 2 or above toxic side effects of oral mucositis.
The results showed that in the observation group (23 cases using MEBO) and the control group (22 cases using compound chlorhexidine gargle), a total of 45 cases were treated for 1-2 weeks. In the observation group, 16 cases were cured, 7 cases improved, with a cure rate of 69.5% and a total effective rate of 100%. In the control group, 9 cases were cured, 10 cases improved, 3 cases were ineffective, with a cure rate of 40.1% and a total effective rate of 86.3%. The conclusion was that MEBO is effective in relieving pain, repairing mucosal tissue, and promoting wound healing in the treatment of tyrosine kinase inhibitor-associated oral mucositis. However, due to the small sample size, further studies with larger sample sizes are needed for verification.