Intrahepatic cholangiocarcinoma (ICC) is the second most common type of primary liver cancer after hepatocellular carcinoma, accounting for 10-15% of all primary liver cancers. It is rightly termed the "second-in-command" of killers within the liver. Over the past 40 years, the incidence of ICC has been rising globally, particularly in Asia.
ICC is highly malignant, and patients are often diagnosed at an advanced stage, making surgical removal minimally effective. However, surgery remains the primary treatment for early-stage ICC, even though the recurrence rate is as high as 60-70% and the prognosis is poor, with a five-year survival rate of only 30%. Given these challenges, clinicians are constantly seeking new treatment methods to improve outcomes for patients.

Case Sharing by Dr. Liu Shupeng, Deputy Director of the Fifth Medical Department
Case Study
Patient Information
A 64-year-old male was admitted to the hospital with a history of progressive weight loss for over three months and a diagnosis of ICC one week prior. The patient had experienced a decrease in appetite and progressive weight loss without any clear cause. A CT scan at an outside hospital revealed a liver mass. A subsequent PET/CT scan and liver biopsy confirmed the diagnosis of intrahepatic cholangiocarcinoma.

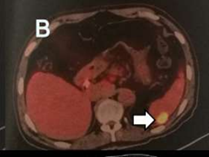
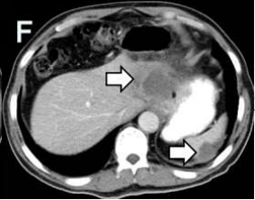
Imaging Examination
Upon further investigation, the liver lesion was found to be adherent to the gastric lesser curvature and diaphragm with indistinct boundaries. The left branch of the portal vein and the left hepatic vein were not visible, suggesting invasion. The anterior and posterior peritoneum of the left upper abdomen showed localized thickening, likely indicating peritoneal metastases. Some lesions were also adherent to the left diaphragm and spleen, with unclear boundaries.
Moreover, tumor markers showed elevated levels: CA19-9 at 259.4 U/ml and CA125 at 103.40 U/ml.
Expert Opinion
After thorough discussion by the expert team, led by Deputy Director Liu Shupeng, it was concluded that the tumor was located in the intrahepatic bile ducts, measuring approximately 7.4 cm x 5.9 cm x 6.2 cm, and was confirmed to be ICC. Following a multidisciplinary consultation, the team determined that the tumor had invaded surrounding tissues and had distant metastases, making the patient ineligible for surgery. Instead, the team proposed a combination of irreversible electroporation (IRE) and chemotherapy for treatment.
Treatment Process
Due to the tumor's invasion of the stomach wall, the patient underwent bowel cleansing with phosphate soda one day before surgery and was instructed to fast and refrain from drinking water for eight hours. A nasogastric tube and urinary catheter were placed 30 minutes before the operation, and 1g of gemcitabine was administered intravenously one hour before surgery.
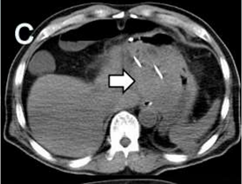
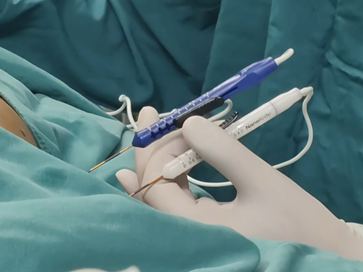
During the procedure, the tumor was localized via CT imaging and punctured under ultrasound guidance through both the abdomen and left chest wall. Two ablation needles were inserted, spaced 2.5 cm apart and parallel to each other, with 2 cm of the needle tips exposed for the ablation process. Due to the large size of the liver tumor, multiple ablation sessions were performed in different sections to ensure complete coverage of the tumor.

Post-Operative Care
After surgery, the patient was started on a liquid diet and given oral tegafur capsules. Post-operative monitoring showed significant necrosis of the liver and peritoneal tumors, with a slight enhancement around the liver tumor's periphery. The patient’s tumor markers significantly decreased, and their weight increased by 4 kg. Pain and daily activity levels also improved notably.
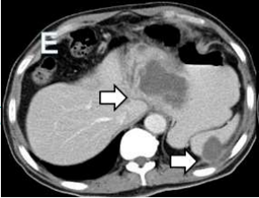
1 week after procedure 2 months after procedure
Irreversible Electroporation (IRE) as a New Option
IRE, a minimally invasive technology, creates a high-intensity electric field to disrupt tumor cell membranes while sparing surrounding healthy tissue, providing a novel treatment option for ICC patients.
Mechanism of Action
IRE works by applying high-voltage pulses to create nanometer-sized pores in the cell membrane, disrupting the exchange of substances inside and outside the cells, ultimately leading to cell death.
Tissue Selectivity and Safety
IRE is highly selective, primarily affecting cell membranes without damaging nearby structures such as blood vessels and nerves. Compared to traditional thermal ablation methods, IRE causes less damage to surrounding healthy tissue during treatment.
Recovery and Complication Risk
Since IRE does not involve high temperatures, the recovery period is shorter, and the risk of complications is lower, making it a relatively safe treatment option, especially for tumors near critical structures like blood vessels, bile ducts, pancreatic ducts, or ureters.
Clinical practice has shown that combining IRE with chemotherapy improves treatment efficacy, reduces side effects, and enhances tumor sensitivity to chemotherapy drugs, leading to better patient outcomes. However, long-term outcomes and quality of life following IRE combined with chemotherapy are not yet fully understood. More clinical studies are needed to refine surgical techniques and optimize drug use, aiming to reduce side effects and improve both treatment safety and patient quality of life.