On June 14, 2024, the American Association for Thoracic Surgery (AATS) released the "Expert Consensus on the Management of Subsolid Pulmonary Nodules." In this consensus, jointly formulated by top thoracic surgery experts worldwide, a research paper titled "Computed tomography-guided percutaneous cryoablation for lung ground-glass opacity: A pilot study," co-authored by Niu Lizhi, President of Guangzhou Fuda Cancer Hospital, and Liu Shupeng, Deputy Director of the hospital's Medical Department V in 2019, was cited as a reference. This citation signifies the recognition and importance of our hospital's research in this field, introducing and promoting it to peers both domestically and internationally through expert consensus.
▲Expert Consensus on the Management of Subsolid Pulmonary Nodules
▲Excerpt
Lung Nodules ≠ Lung Cancer
Lung nodules do not equate to lung cancer; many diseases can form pulmonary nodules, with approximately 90% being benign, such as inflammation, tuberculoma, granuloma, lung abscess, hamartoma, and fungal ball. However, vigilance is crucial because a certain percentage of nodules are early-stage lung cancer, making regular check-ups essential. Some benign lesions may also transform into malignancies over time.
When lung nodules are detected, patients often wish for a definitive answer on whether they are benign or malignant. Doctors will use their experience for differential diagnosis, recommending "high vigilance and surgery if necessary" if malignancy is suspected. The most valuable recommendation for most pulmonary nodules is regular follow-up examinations to observe changes dynamically, with intervals based on nodule size, preferably at the same hospital for accurate comparisons.
Not all patients with lung nodules can undergo surgery. For those unable to undergo surgery due to advanced age, poor cardiopulmonary function, multiple lung nodules, or postoperative recurrence and metastasis, cryoablation is a good alternative. In our hospital's study, 19 subsolid nodules in 14 patients underwent cryoablation, all of which were completely ablated within a median follow-up of 24 months, achieving a technical success rate of 100%, with no cryoablation-related deaths.
▲Fuda’s Published Paper
Understanding Cryoablation
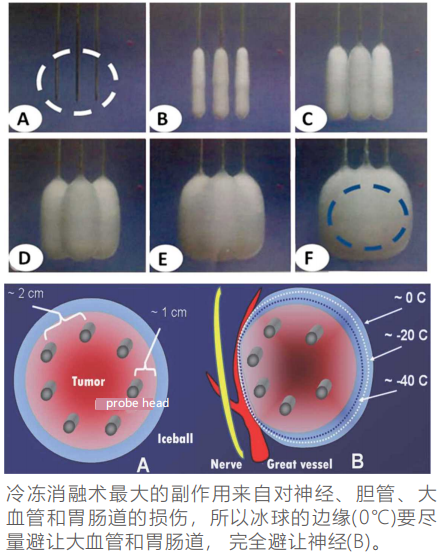
Cryoablation therapy combines ultra-low temperature freezing at -140°C to -190°C, tumor destruction without surgery, and immune enhancement. The basic principle is rapid freezing of cancerous tissue to form an ice ball, followed by thawing, leading to further cancer cell necrosis or apoptosis, achieving ablation. For smaller tumors, the probe can be directly inserted into the tumor center from any angle; for larger tumors, multiple cryoprobes are used simultaneously, following a designed program for insertion.

The most notable feature of cryoablation is the formation of a clearly visible ice ball under ultrasound or CT. During ablation, the probe is directly inserted into the tumor through the skin, lowering the tissue temperature to -160°C, forming small ice balls that gradually merge into a larger one, completely covering the tumor. During the thawing process, the temperature of the diseased tissue quickly rises to 40°C. Repeating this cycle ensures thorough tumor destruction.
Currently, China's cryoablation technology leads the world. As the chair unit of the International Society of Cryosurgery and the Asia-Pacific Tumor Cryoablation Training Center, Guangzhou Fuda Cancer Hospital has used cryoablation technology to treat dozens of cancer types, with tens of thousands of cases, publishing numerous related papers and authoring the Chinese-English book "Modern Cryosurgery For Cancer." This extensive clinical experience has attracted doctors from South Korea, Malaysia, Indonesia, the Philippines, Taiwan, Hong Kong, and mainland China for training at Fuda. The hospital has received the "Special Contribution Award in World Cryosurgery," the "Outstanding Contribution Award" at the World Tumor Interventional Conference, and the "Outstanding Contribution Award" at the Chinese Academic Conference on Minimally Invasive Oncology.