On October 12-13, 2024, the 10th Asian Conference on Tumor Ablation (ACTA) was grandly held in Bali, Indonesia.
ACTA serves as the annual forum for Asian tumor ablation experts. Since its inaugural session in 2014, it has evolved into one of the largest and most academically influential conferences in the field of ablation, garnering widespread attention and attracting global participation to promote new advancements and achievements in tumor ablation research.

The theme of this year's conference was “Toward a Perfect Tumor Ablation.” Experts and researchers from countries including China, Indonesia, South Korea, Japan, the USA, Taiwan, Singapore, the Philippines, and Malaysia gathered to discuss the latest developments in tumor ablation.
Niu Lizhi, President of Guangzhou Fuda Cancer Hospital, along with Yang Yang from the central laboratory and Liu Zhengping, head of the Fuda Indonesia office, were invited. Prof. Niu led the team in presenting their findings on "Chemotherapy plus IRE improved local tumor control in unresectable hilar cholangiocarcinoma," which received positive feedback from attendees, ultimately earning them a second-place award for outstanding presentation.

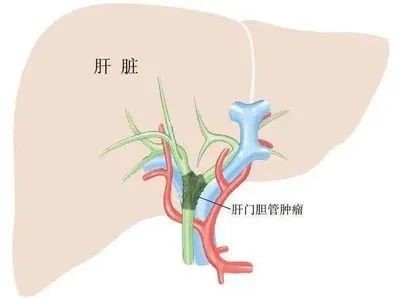
Hilar cholangiocarcinoma, also known as Klatskin tumor, accounts for approximately 50%-70% of all bile duct cancers, occurring at the junction of the left and right hepatic ducts. It is highly malignant with poor prognosis. Surgery is the only potentially curative treatment, but most patients are diagnosed at advanced stages, complicating surgical intervention or making it impossible. Recurrence, particularly local recurrence (about 83%), significantly impacts survival.
The standard treatment for unresectable hilar cholangiocarcinoma (UHC) is palliative chemotherapy, with a median overall survival of around 12 months. However, 70% of patients undergoing chemotherapy experience grade 3 or higher toxicity, and their quality of life is severely affected due to jaundice and complications from long-term drainage or recurrent infections. Thus, addressing the need for tumor downstaging, progression delay, survival extension, and quality of life improvement is crucial.
Current treatments include chemotherapy, radiotherapy, biliary drainage, photodynamic therapy, radiofrequency ablation, targeted therapy, and immunotherapy. These methods have improved patient outcomes to varying degrees, but the proximity of tumors to bile ducts and hepatic vessels raises the risk of complications such as obstruction, strictures, leaks, bleeding, and thrombosis.
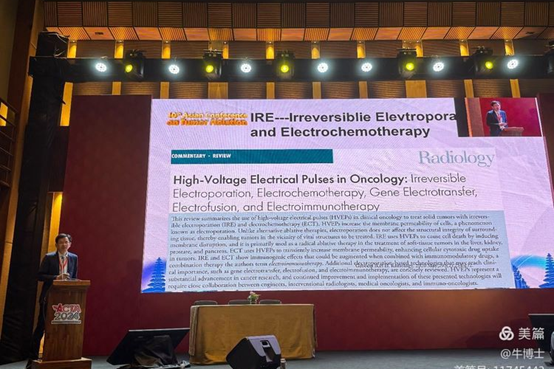
NanoKnife ablation (IRE), a novel non-thermal ablation technique, employs irreversible electroporation to disrupt cell membranes with short, high-voltage pulses, causing permanent damage and apoptosis in tumor cells while sparing surrounding structures. This positions IRE as a theoretically safe and effective option for tumors adjacent to critical structures. As of September 2024, Guangzhou Fuda Cancer Hospital has performed 1,058 IRE procedures, accumulating extensive clinical experience.

Clinical studies have shown promising results with the combination of NanoKnife and chemotherapy for UHC. Recent literature reviews and meta-analyses, such as that by Professor Anna from the University of Rome, indicate that the average survival for patients undergoing NanoKnife with chemotherapy is 25 months, significantly higher than previous averages for surgery (29.6 months) and chemotherapy alone (12.2 months).
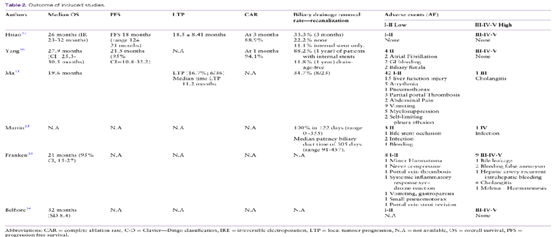
The Guangzhou Fuda Cancer Hospital team also designed a study combining chemotherapy with NanoKnife ablation for UHC treatment. They divided 47 UHC patients into a chemotherapy + IRE group (n=23) and a chemotherapy-only group (n=24), with no treatment-related deaths reported.
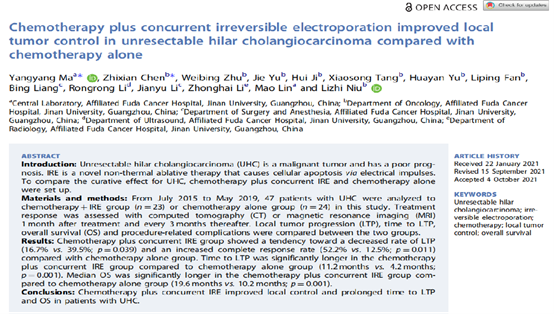
Results indicated a decreasing trend in local tumor progression (16.7% vs. 39.5%; p=0.039) and an increased complete response rate (52.2% vs. 12.5%; p=0.011) in the chemotherapy + IRE group. Additionally, the median overall survival was significantly longer in the combination group (19.6 months vs. 10.2 months; p<0.001).
Clearly, the combination of chemotherapy with IRE shows superior efficacy compared to chemotherapy alone in terms of local control rates, progression-free survival, and overall survival. However, this study has limitations, particularly regarding the small sample size, necessitating multi-center and larger studies for validation.