Wang (a pseudonym), from Hunan, discovered a mass in her abdomen two years ago, which could be moved by touch. Concerned, she consulted her friend, only to realize that this could be an abnormal sign when she was told her friend had no similar issue. After checking with a local hospital, she was diagnosed with a tumor.
On the advice of the local doctor, Wang underwent surgery for tumor removal. The postoperative pathology confirmed a diagnosis of uterine perivascular epithelioid cell tumor (PEComa). She then completed six cycles of adjuvant chemotherapy, during which the follow-up results were relatively stable. However, in March 2024, a new soft tissue mass was found behind her right peritoneum. As the tumor grew, her abdomen also enlarged. CT scans suggested the likelihood of metastatic tumors, with multiple lymph node metastases in the liver hilum and retroperitoneum.
Less than a year after surgery, the tumor recurred and metastasized, which was a huge blow to Wang and her family. Due to the size of the tumor and the complexity of the surgery, even after undergoing a second surgery locally, only part of the tumor was removed, and complete removal was not possible. Within just half a month after the surgery, the tumor had grown to approximately 15 cm. This surgery clarified the tumor's nature—suspected to be malignant perivascular epithelioid cell tumor (PEComa). The tumor's progression also caused Wang continuous symptoms, including coughing, shortness of breath, vomiting, and pain, severely affecting her physical and mental health.
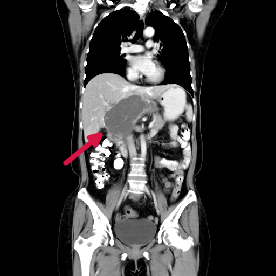
Despite these setbacks, Wang did not give up. Her spouse continued to actively search for specialized cancer hospitals to find new treatment options. After much inquiry, they finally came to the Guangzhou Fuda Cancer Hospital, a national clinical oncology center, in July 2024. Upon admission, Wang was unable to eat and would vomit immediately after eating. Enhanced CT scans showed that the tumor had grown to about 22 cm and was pressing on her stomach, narrowing the gastric cavity.
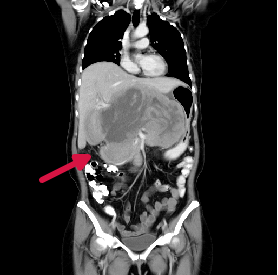
Pre-Treatment Imaging
Given Wang's situation, Dr. Li Hongmei, Deputy Director of the Medical Six Department, immediately initiated a multidisciplinary consultation. Due to the large size of the retroperitoneal tumor, which had recurred after two surgeries, there was no possibility for radical resection. After consulting with Wang and her family, Dr. Li formulated an interventional therapy plan targeting the retroperitoneal tumor, combined with targeted drug therapy.
During the procedure, DSA imaging revealed that the tumor had abundant blood supply and had invaded the liver. After analyzing the results, Dr. Yang Qingfeng, Deputy Director of the Interventional Department, determined that the main blood supply to the tumor likely came from the hepatic artery. Under DSA guidance, he selectively embolized the left, middle, and right hepatic arteries, which were the tumor's main blood vessels, and performed transcatheter arterial chemoembolization (TACE) via the femoral artery. This treatment aimed to block the tumor's nutrient supply, starving and killing the tumor cells.
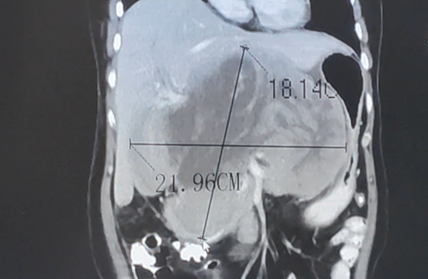
Before treatment
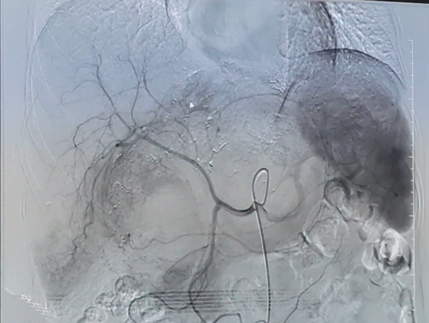
The tumor had rich blood supply
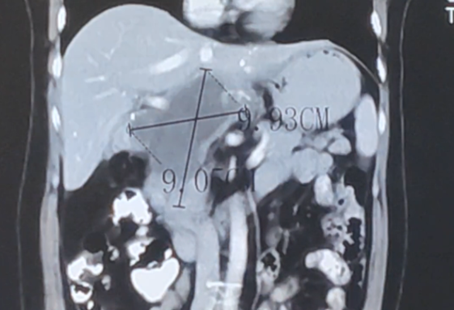
The tumor shrank, and multiple areas of necrosis appeared
After the first session of treatment, Wang's nausea and vomiting significantly improved. Following the second session, imaging results showed an 80% reduction in the tumor size with notable necrosis, and her gastric cavity gradually returned to normal. "Compared to open surgery, the interventional treatment is much easier," she remarked. With each successive interventional treatment, Wang's condition improved progressively.
Post-Treatment
By early December 2024, after four rounds of interventional therapy, follow-up results showed the tumor had shrunk by about 80%. Wang’s vomiting and nausea had completely resolved, and she had gained 5 kilograms. Now, aside from taking oral targeted drugs and having regular check-ups, Wang lives a normal life, occasionally playing cards and taking care of her child, which she is very satisfied with.
Uterine Perivascular Epithelioid Cell Tumor (PEComa)
Uterine sarcomas include leiomyosarcoma, endometrial stromal sarcoma, undifferentiated sarcoma, and rare types like rhabdomyosarcoma and malignant perivascular epithelioid cell tumor (PEComa), with the latter being very uncommon in the uterus. It predominantly occurs in women aged 40-60 years, and factors like gene expression and estrogen receptor presence may play a role. Some uterine sarcomas may develop secondary to uterine leiomyomas.
PEComa is a rare mesenchymal tumor composed of perivascular epithelioid cells, characterized by unique immunohistochemical markers. The tumor cells show local association with the vascular wall and usually express melanocytic and smooth muscle markers. PEComas occurring in the uterus are extremely rare, with few reported cases. The cause remains unclear, though some PEComas are associated with mutations in the tuberous sclerosis complex (TSC) gene. Clinical manifestations are non-specific, including abnormal uterine bleeding, abdominal and pelvic masses, and imaging findings similar to uterine fibroids.
Current classification divides the tumor into benign, malignant potential uncertain, and malignant:
- **Benign**: < 5 cm, no expansive growth, no vascular invasion, low nuclear grade, mitotic index ≤ 1/50mm²
- **Uncertain malignant potential**: Tumors larger than 5 cm or exhibiting nuclear abnormalities or multinucleated giant cells.
- **Malignant**: Tumors with at least two malignant features or three according to modified gynecological standards (e.g., > 5 cm, expansive growth, high-grade nuclei, mitotic index > 1/50mm², necrosis, vascular invasion).
It is worth noting that even benign tumors have the potential for malignant transformation over time.
Due to the lack of treatment guidelines for gynecological PEComas, surgery remains the primary treatment modality. The surgical approach is tailored to the patient's condition. For high-risk cases, adjuvant therapy may be necessary post-surgery, although long-term outcomes remain uncertain due to the rarity of such cases.
