Tumor Progresses After Chemotherapy
Uncle Jin, 66 years old (a pseudonym), from Shanxi, was diagnosed with pulmonary interstitial fibrosis five years ago. This past New Year, Uncle Jin began coughing and coughing up phlegm with traces of blood. Realizing something was wrong, he went to a local hospital with his children. The final diagnosis was: small-cell lung cancer of the right lung, in the limited stage.
Despite eating and working like a normal person, and having annual physical check-ups with no major issues, he had been on medication for pulmonary fibrosis regularly. How could this happen to him? Fearing the emotional burden on Uncle Jin, his children kept the diagnosis hidden from him. It wasn’t until he returned home after his hospitalization and started packing his suitcase that he found the report. With an incredibly positive attitude, he didn’t lose heart but made one request: "Don't let your mother know, as she's in poor health."
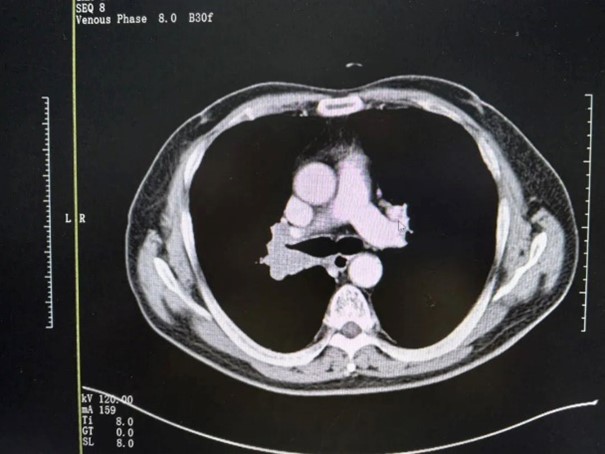
So, Uncle Jin quietly began chemotherapy at the local hospital. However, after six rounds of treatment, the tumor not only failed to shrink but had actually grown. There was also metastasis to the right lung hilum and mediastinal lymph nodes, along with solid nodules in the lungs. This made Uncle Jin feel that he had taken the wrong path. But he didn’t give up and continued to seek out medical advice.
Trust in Fuda
After hearing about other treatment options, Uncle Jin arrived at the Fuda Cancer Hospital in Guangzhou’s Medical Oncology Department in late July 2024. Despite being in a non-public hospital, even while sitting in the hospital’s café waiting to complete the paperwork, his children were still in contact with other major hospitals in Guangzhou. Nevertheless, Uncle Jin was adamant about staying at Fuda, saying, "My intuition told me to trust this hospital."
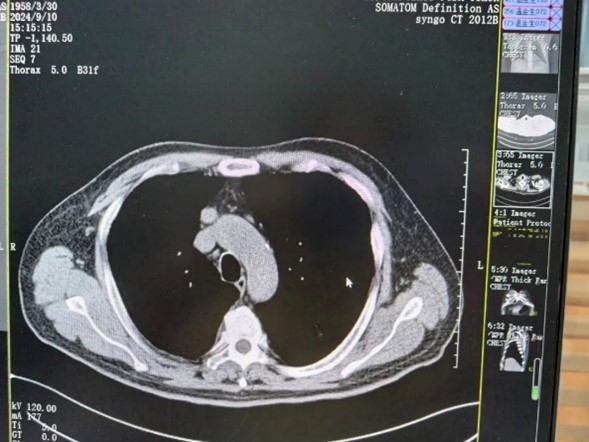
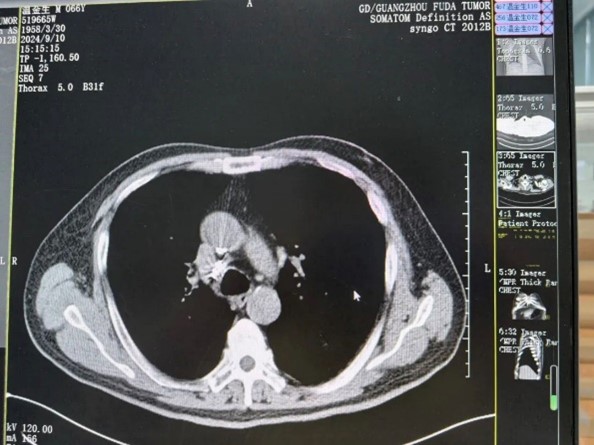
Upon examination, it was found that Uncle Jin had a 4.3x3.8x2.5 cm mass in the right lung hilum, with adjacent bronchial compression and narrowing. Multiple ground-glass nodules were seen in both lungs, and there were multiple enlarged lymph nodes in the mediastinum and right lung hilum, with the largest being 3.4x2.4 cm. Based on his medical history and clinical results, Dr. Shi Haiyan from the Medical Oncology Department immediately requested a multidisciplinary team consultation. After evaluation, it was determined that due to the slow progression of the small-cell lung cancer and the proximity of the tumor to major blood vessels, surgery posed a high risk. Therefore, the team recommended local treatment such as radiation therapy, as well as a change in the systemic anti-tumor regimen.

Particle Implantation + Interventional Therapy + Immunotherapy = Positive Outcome
Although Uncle Jin and his family initially rejected conventional radiation therapy, they later agreed on a treatment plan that included iodine-125 particle implantation for the right lung tumor and mediastinal lymph node metastasis, along with arterial infusion chemotherapy and combined immunotherapy.
Radioactive particle implantation has the advantage of delivering a high dose to the tumor while minimizing damage to surrounding normal tissue. It is effective for treating tumors that are inoperable or have recurred after other treatments, including metastasis to the mediastinal lymph nodes, often referred to as the “corner of death.” Additionally, through digital subtraction angiography (DSA), chemotherapy drugs were directly infused into the tumor’s blood supply artery, increasing the local drug concentration and effectively killing tumor tissue. Meanwhile, systemic treatment was provided with PD-1 immunotherapy to control tumor progression.

After undergoing one round of particle implantation and three or four cycles of interventional and immunotherapy treatments, Uncle Jin truly felt that his initial "intuition" was correct. Each treatment was better than the last. His CT scans showed that the tumor in the right lung hilum had clearly shrunk, and the enlarged lymph nodes in the mediastinum, as well as some of the nodules in both lungs, had also reduced in size. Throughout his multiple hospital stays, Uncle Jin experienced the best medical care he had ever received.
Because he did not undergo major surgery, Uncle Jin did not experience significant discomfort. Even when receiving interventional treatment, it was done in a comfortable and conversational manner with the medical staff. “Everyone, from the nurses to the department heads, treated me with warmth and care. I really felt well looked after.”

Staying Positive for Future Hope
For Uncle Jin, who has been diagnosed with cancer, this is just the beginning. He will need to continue maintenance treatments and regular follow-ups. Therefore, maintaining a positive mindset is essential. He has also learned how to prevent the recurrence of cancer. After being diagnosed with pulmonary fibrosis, Uncle Jin immediately quit smoking and drinking, habits he had for over 40 years. Upon his cancer diagnosis, he strictly followed a regimen of "controlling his diet, staying active, sleeping well, and keeping a calm heart." He enjoys regular walks and chats, and his positive attitude has influenced many other patients to join him. He firmly believes that only by maintaining a mindset of victory can he find a way to survive on this difficult journey.
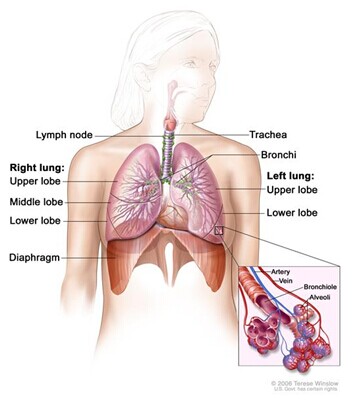
Health Knowledge: Pulmonary Fibrosis and Lung Cancer
Pulmonary interstitial fibrosis is a heterogeneous, chronic scarring disease and is the most common type of interstitial pneumonia. Pathologically, it manifests as usual interstitial pneumonia and progresses over time, often leading to lung cancer.
Lung cancer originates from the bronchial mucosa or glands and is known as bronchial lung cancer. It has a high incidence rate and continues to rise. Studies have shown that patients with pulmonary fibrosis are at a significantly higher risk of developing lung cancer compared to those without it. For example, a meta-analysis by Li J and colleagues found that the incidence of lung cancer in patients with pulmonary fibrosis ranged from 4.8% to 48%, compared to just 2.0% to 6.4% in those without fibrosis.
Current research results indicate that the incidence of lung cancer in patients with pulmonary fibrosis varies by country, region, and population. In the United States, the incidence is 4.8% to 8.0%, while in Japan, it is 48.2%, and in Korea, it is 13.1%. A large-scale domestic meta-analysis shows that the incidence of lung cancer in patients with idiopathic pulmonary fibrosis averages 14%, which is five times higher than in the general population. Among these patients, 90% are male, and the male-to-female ratio is approximately 9:1, with the average age of onset being over 65 years.