Lymphoma is a type of blood cancer that occurs when B or T lymphocytes,[1] the white blood cells that form a part of the immune system and help protect the body from infection and disease, divide faster than normal cells or live longer than they are supposed to. Lymphoma may develop in the lymph nodes, spleen, bone marrow, blood or other organs[2] and eventually they form a tumor.[1]
Typically, lymphoma presents as a solid tumor of lymphoid cells. Treatment might involve chemotherapy and in some cases radiotherapy and/or bone marrow transplantation, and lymphomas can be curable depending on the histology, type, and stage of the disease.[3] These malignant cells often originate in lymph nodes, presenting as an enlargement of the node (a tumor). It can also affect other organs in which case it is referred to as extranodal lymphoma. Extranodal sites include the skin, brain, bowels and bone. Lymphomas are closely related to lymphoid leukemias, which also originate in lymphocytes but typically involve only circulating blood and the bone marrow (where blood cells are generated in a process termed haematopoesis) and do not usually form static tumors.[3] There are many types of lymphomas, and in turn, lymphomas are a part of the broad group of diseases called hematological neoplasms.
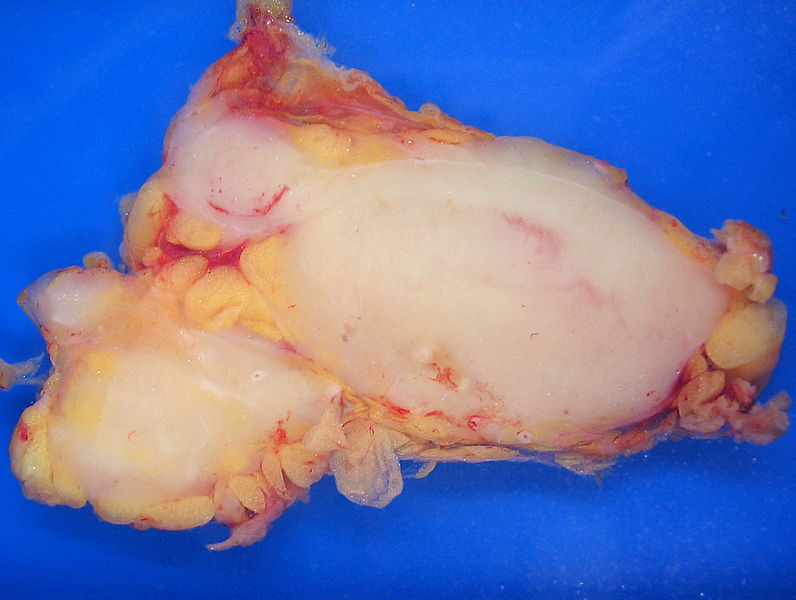
Follicular lymphoma replacing a lymph node
Lymphoma and lymphatic system
Signs and symptoms
Lymphoma presents with certain non-specific symptoms. If symptoms are persistent, lymphoma needs to be excluded medically.
Lymphadenopathy[2][4] or swelling of lymph nodes – It is the primary presentation in lymphoma.
B symptoms (systemic symptoms) – Can be associated with both Hodgkin's lymphoma and non-Hodgkin's lymphoma. They consist of:
Fever[2][4]
Night sweats[2][4]
Weight loss[2][4]
Other Symptoms :
Loss of appetite or anorexia[4]
Fatigue[2][4]
Respiratory distress or dyspnoea[4]
Itching[2][4]
Diagnosis
Lymphoma is definitively diagnosed by a lymph node biopsy, meaning a partial or total excision of a lymph node that is then examined under the microscope.[5] This examination reveals histopathologicalfeatures that may indicate lymphoma. After lymphoma is diagnosed, a variety of tests may be carried out to look for specific features characteristic of different types of lymphoma. These include:
Immunophenotyping
Flow cytometry
FISH testing.
Several classification systems have existed for lymphoma. These systems use histological findings and other findings to divide lymphoma into different categories. The classification of lymphoma can affect treatment and prognosis. Classification systems generally classify lymphoma according to:
Whether or not it is a Hodgkin lymphoma.
Whether the cell that is replicating is a T cell or B cell.
The site that the cell arises from.
Hodgkin's lymphoma
Main article: Hodgkin's lymphoma
Hodgkin's lymphoma is one of the most well-known types of lymphoma,[citation needed] and differs from other forms of lymphoma in its prognosis and several pathological characteristics. A division into Hodgkin's and non-Hodgkin's lymphomas is used in several formal classification systems. A Hodgkin's lymphoma is marked by the presence of a type of cell called the Reed-Sternberg cell.[6][7]
WHO classification
The current accepted definition is the WHO classification, published in 2001 and updated in 2008,[8][9] is the latest classification of lymphoma and is based upon the foundations laid within the "Revised European-American Lymphoma classification" (REAL). This system attempts to group lymphomas by cell type (i.e. the normal cell type that most resembles the tumor) and defining phenotypic, molecular or cytogenetic characteristics. There are three large groups: the B cell, T cell, and natural killer cell tumors. Other less common groups, are also recognized. Hodgkin lymphoma, although considered separately within the World Health Organization (and preceding) classifications, is now recognized as being a tumor of, albeit markedly abnormal, lymphocytes of mature B cell lineage.
Subtypes according to the WHO classification
Mature B-cell neoplasms [show]
Mature T cell and natural killer (NK) cell neoplasms [show]
Hodgkin Lymphoma [show]
Immunodeficiency-associated lymphoproliferative disorders [show]
Working Formulation
Main article: Working Formulation
The 1996 Working Formulation was a classification of non-Hodgkin lymphoma. It excluded the Hodgkin lymphomas and divided the remaining lymphomas into four grades (Low, Intermediate, High, and Miscellaneous) related to prognosis, with some further subdivisions based on the size and shape of affected cells. This purely histological classification included no information about cell surface markers, or genetics, and it made no distinction between T-cell lymphomas or B-cell lymphomas. It was widely accepted at the time of its publication but is now obsolete.[10] It is still used by some cancer agencies for compilation of lymphoma statistics and historical rate comparisons.[citation needed]
Other
REAL. In the mid 1990s, the Revised European-American Lymphoma (REAL) Classification attempted to apply immunophenotypic and genetic features in identifying distinct clinicopathologic entities among all the lymphomas except Hodgkin's lymphoma.[11]
ICD-O (codes 9590–9999, details at [2])
ICD-10 (codes C81-C96, details at [3])
Subtypes
There are many forms of lymphoma. Some forms of lymphoma are categorized as indolent (e.g. small lymphocytic lymphoma), compatible with a long life even without treatment, whereas other forms are aggressive (e.g. Burkitt's lymphoma), causing rapid deterioration and death. However, most of the aggressive lymphomas respond well to treatment and are curable. The prognosis therefore depends on the correct diagnosis and classification of the disease, which is established after examination of a biopsy by a pathologist (usually a hematopathologist).[12]
Lymphoma subtypes.[13]
| Lymphoma type | Relativeincidence[13] | Histopathology [13] | Immunophenotype | Overall 5-year survival | Other comments[13] |
|---|---|---|---|---|---|
| Precursor T-cell leukemia/lymphoma | 40% of lymphomas in childhood. | Lymphoblasts with irregular nuclear contours, condensed chromatin, small nucleoli and scant cytoplasm without granules. | TdT, CD2, CD7 | It often presents as a mediastinal mass because of involvement of the thymus. It is highly associated with NOTCH1mutations. Most common inadolescent males. | |
| Follicular lymphoma | 40% of lymphomas in adults | Small "cleaved" cells (centrocytes) mixed with large activated cells (centroblasts). Usually nodular ("follicular") growth pattern | CD10, surface Ig | 72–77%[14] | Occurs in older adults. Usually involves lymph nodes, bone marrow and spleen. Associated with t(14;18)translocationoverexpressingBcl-2. Indolent |
| Diffuse large B cell lymphoma | 40 to 50% of lymphomas in adults | Variable. Most resemble B cells of large germinal centers. Diffuse growth pattern. | Variable expression ofCD10 and surface Ig | 60%[15] | Occurs in all ages, but most commonly in older adults. Often occurs outside lymph nodes. Aggressive. |
| Mantle cell lymphoma | 3 to 4% of lymphomas in adults | Lymphocytes of small to intermediate size growing in diffuse pattern | CD5 | 50%[16]to 70%[16] | Occurs mainly in adult males. Usually involves lymph nodes, bone marrow, spleen and GI tract. Associated with t(11;14) translocation overexpressingcyclin D1. Moderately aggressive. |
| B-cell chronic lymphocytic leukemia/lymphoma | 3 to 4% of lymphomas in adults | Small resting lymphocytes mixed with variable number of large activated cells. Lymph nodes are diffusely effaced | CD5, surfaceimmunoglobulin | 50%.[17] | Occurs in older adults. Usually involves lymph nodes, bone marrow and spleen. Most patients have peripheral blood involvement.Indolent. |
| MALT lymphoma | ~5% of lymphomas in adults | Variable cell size and differentiation. 40% showplasma celldifferentiation. Homingof B cells to epithelium creates lymphoepithelial lesions. | CD5, CD10, surface Ig | Frequently occurs outside lymph nodes. Very indolent. May be cured by local excision. | |
| Burkitt's lymphoma | < 1% of lymphomas in the United States | Round lymphoid cells of intermediate size with several nucleoli. Starry-sky appearance by diffuse spread with interspersedapoptosis. | CD10, surface Ig | 50%[18] | Endemic in Africa, sporadic elsewhere. More common in immunocompromised and in children. Often visceral involvement. Highly aggressive. |
| Mycosis fungoides | Most common cutaneous lymphoid malignancy | Usually small lymphoid cells with convoluted nuclei that often infiltrate the epidermis, creating Pautier microabscesses. | CD4 | 75%[19] | Localized or more generalized skin symptoms. Generally indolent. In a more aggressive variant, Sézary's disease, there is skin erythema and peripheral blood involvement. |
| Peripheral T-cell lymphoma-Not-Otherwise-Specified | Most common T cell lymphoma | Variable. Usually a mix small to large lymphoid cells with irregular nuclear contours. | CD3 | Probably consists of several rare tumor types. It is often disseminated and generally aggressive. | |
| Nodular sclerosisform of Hodgkin lymphoma | Most common type of Hodgkin's lymphoma | Reed-Sternberg cellvariants and inflammation. usually broad sclerotic bands that consists of collagen. | CD15, CD30 | Most common in young adults. It often arises in the mediastinumor cervical lymph nodes. | |
| Mixed-cellularity subtype ofHodgkin lymphoma | Second most common form of Hodgkin's lymphoma | Many classic Reed-Sternberg cells and inflammation | CD15, CD30 | Most common in men. More likely to be diagnosed at advanced stages than the nodular sclerosis form. Epstein-Barr virusinvolved in 70% of cases. |
Staging
After a diagnosis and before treatment, a cancer is staged. This refers to deducing how far the cancer has spread, in local tissue and to other sites. Staging is reported as a grade between I (confined) and IV (spread). Staging is carried out because the stage of a cancer impacts its prognosis and treatment.[citation needed]
The Ann Arbor staging system is routinely used for staging of both HL and NHL. In this staging system, I represents a localised disease contained within a lymph node, II the presence of lymphoma in two or more lymph nodes, III spread of the lymphoma to both sides of thediaphragm, and IV to tissue outside a lymph node.[citation needed]
A CT scan or PET scan are imaging modalities used to stage a cancer.[citation needed]
Treatment
Prognosis and treatment is different for HL and between all the different forms of NHL,[20] and also depends on the grade of tumour, referring to how quickly a cancer replicates. Paradoxically, high-grade lymphomas are more readily treated and have better prognoses[citation needed]. A well-known example of a high-grade tumour is that of Burkitt's lymphoma, which is a high-grade tumour that has been known to double within days, but is readily treated.
Low-grade lymphomas
Many low-grade lymphomas remain indolent for many years. In these lymphomas, metastases are very likely. For this reason, treatment of the non-symptomatic patient is often avoided. In these forms of lymphoma[which?], watchful waiting is often the initial course of action. This is carried out because the harms and risks of treatment outweigh the benefits.[21] If a low-grade lymphoma is becoming symptomatic, radiotherapy or chemotherapy are the treatments of choice; although they do not cure the lymphoma, they can alleviate the symptoms, particularly painful lymphadenopathy. Patients with these types of lymphoma can live near-normal lifespans, but the disease is incurable.
High-grade lymphomas
Treatment of some other, more aggressive, forms of lymphoma[which?]can result in a cure in the majority of cases, but the prognosis for patients with a poor response to therapy is worse.[22] Treatment for these types of lymphoma typically consists of aggressive chemotherapy, including the CHOP or R-CHOP regimen.
Hodgkin lymphoma typically is treated with radiotherapy alone, as long as it is localized.[23] Advanced Hodgkin disease requires systemic chemotherapy, sometimes combined with radiotherapy.[24]Chemotherapy used includes the ABVD regimen.
Prognosis
| 5-year relative survival by stage at diagnosis[25] | ||
|---|---|---|
| Stage at diagnosis | 5-year relative survival (%) | Percentage of cases (%) |
| Localized (confined to primary site) | 82.1 | 27 |
| Regional (spread to regional lymph nodes) | 77.5 | 19 |
| Distant (cancer has metastasized) | 59.9 | 45 |
| Unknown (unstaged) | 67.5 | 9 |
Epidemiology
Lymphoma is the most common form of hematological malignancy, or "blood cancer", in the developed world.
Taken together, lymphomas represent 5.3% of all cancers (excluding simple basal cell and squamous cell skin cancers) in the United States and 55.6% of all blood cancers.[27]
According to the U.S. National Institutes of Health, lymphomas account for about five percent of all cases of cancer in the United States, and Hodgkin's lymphoma in particular accounts for less than one percent of all cases of cancer in the United States.
Because the whole system is part of the body's immune system, patients with a weakened immune system such as from HIV infection or from certain drugs or medication also have a higher incidence of lymphoma.
History
Thomas Hodgkin published the first description of lymphoma in 1832, specifically of the form named after him, Hodgkin's lymphoma.[28]Since then, many other forms of lymphoma have been described, grouped under several proposed classifications. The 1982 Working formulation became very popular. It introduced the category non-Hodgkin lymphoma, divided into 16 diseases. However, because these lymphomas have little in common with each other, the NHL label is of limited usefulness for doctors or patients and is slowly being abandoned. The latest classification by the WHO (2008) lists 70 forms of lymphoma divided into four broad groups.[8]
As an alternative to the American Lakes-Butler classification, in the early 1970s, Karl Lennert ofKiel, Germany, proposed a new system of classifying lymphomas based on cellular morphology and their relationship to cells of the normal peripheral lymphoid system.[29]
Research directions
Significant research into the causes, prevalence, diagnosis, treatment, and prognosis of lymphoma is being performed. Hundreds of clinical trials are being planned or conducted at any given time.[30]Studies may focus on effective means of treatment, better ways of treating the disease, improving the quality of life for patients, or appropriate care in remission or after cures.
In general, there are two types of lymphoma research: clinical or translational research and basic research. Clinical/translational research focuses on studying the disease in a defined and generally immediately patient-applicable way, such as testing a new drug in patients. By contrast, basic science research studies the disease process at a distance, such as seeing whether a suspected carcinogen can cause healthy cells to turn into lymphoma cells in the laboratory or how the DNA changes inside lymphoma cells as the disease progresses. The results from basic research studies are generally less immediately useful to patients with the disease[31] but can improve scientists' understanding of lymphoma and form the foundation for future, more effective treatments.
References
1. :a b "What is lymphoma?". Medical News Today. Retrieved 28 February 2013.
2. :a b c d e f g "About Lymphoma". Lymphoma Research Foundation. Retrieved 22 December 2012.
3. :a b Parham, Peter (2005). The immune system. New York: Garland Science. p. 414. ISBN 0-8153-4093-1.
4. :a b c d e f g h "Warning Signs of Lymphoma — First Signs of Lymphoma". Lymphoma.about.com. Retrieved 2012-12-01.
5. Mallick, Indranil. "How Is Lymphoma Diagnosed?". lymphoma.about.com. Retrieved 22 December 2012.
6. National Cancer Institute, "Hodgkin Lymphoma", http://www.cancer.gov/cancertopics/types/hodgkin, accessed on 2013-08-05
7. National Cancer Institute. "What You Need To Know About Hodgkin Lymphoma". U.S. Dept of Health and Human Services, (online at http://www.cancer.gov/cancertopics/wyntk/hodgkin.pdf), pg 4.
8. :a b Swerdlow, Steven H.; International Agency for Research on Cancer; World Health Organization (2008). WHO classification of tumours of haematopoietic and lymphoid tissues. World Health Organization classification of tumours 2 (4th ed.). International Agency for Research on Cancer. ISBN 9789283224310.
9. Jaffe, Elaine Sarkin (2001). Pathology & Genetics: Tumours of Haematopoietic and Lymphoid Tissues. WHO classification of tumours, pathology and genetics series 3. IARC. ISBN 978-92-832-2411-2.
10. Clarke CA, Glaser SL, Dorfman and Dorfwoman RF, Bracci PM, Eberle E, Holly EA (January 2004). "Expert review of non-Hodgkin lymphomas in a population-based cancer registry: reliability of diagnosis and subtype classifications". Cancer Epidemiol. Bio-markers Prev. 13 (1): 138–43. doi:10.1158/1055-9965.EPI-03-0250.PMID 14744745.
11. Non-Hodgkin Lymphoma at eMedicine
12. Wagman LD. (2008). "Principles of Surgical Oncology". In Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ.Cancer Management: A Multidisciplinary Approach (11th ed.). CMPMedica. ISBN 9781891483622.
13. :a b c d Robbins basic pathology (8th ed.). Philadelphia: Saunders/Elsevier. 2007. pp. Table 12–8. ISBN 1-4160-2973-7.
14. Lymphoma, Follicular at eMedicine
15. Turgeon, Mary Louise (2005). Clinical Hematology: Theory and Procedures 936 (4 ed.). Lippincott Williams & Wilkins. pp. 285–6. ISBN 978-0-7817-5007-3.
16. :a b
◦50% for limited stage, according to: Leitch HA, Gascoyne RD, Chhanabhai M, Voss NJ, Klasa R, Connors JM (October 2003). "Limited-stage mantle-cell lymphoma". Ann. Oncol. 14 (10): 1555–61.doi:10.1093/annonc/mdg414. PMID 14504058.
◦70% for advanced stage, according to most recent values in: Herrmann A, Hoster E, Zwingers T, et al.(February 2009). "Improvement of overall survival in advanced stage mantle cell lymphoma". J. Clin. Oncol.27 (4): 511–8. doi:10.1200/JCO.2008.16.8435. PMID 19075279.
17. "Chronic Leukemias". The Merck Manual of Geriatrics.
18. Diviné M, Casassus P, Koscielny S, et al. (December 2005). "Burkitt lymphoma in adults: a prospective study of 72 patients treated with an adapted pediatric LMB protocol". Ann. Oncol. 16 (12): 1928–35.doi:10.1093/annonc/mdi403. PMID 16284057.
19. Kirova YM, Piedbois Y, Haddad E, et al. (May 1999). "Radiotherapy in the management of mycosis fungoides: indications, results, prognosis. Twenty years experience". Radiother Oncol 51 (2): 147–51. doi:10.1016/S0167-8140(99)00050-X. PMID 10435806.
20. Sweetenham JW (November 2009). "Treatment of lymphoblastic lymphoma in adults". Oncology (Williston Park, N.Y.) 23 (12): 1015–20. PMID 20017283.
21. Elphee EE (May 2008). "Understanding the concept of uncertainty in patients with indolent lymphoma". Oncol Nurs Forum 35 (3): 449–54. doi:10.1188/08.ONF.449-454. PMID 18467294.
22. Bernstein SH, Burack WR (2009). "The incidence, natural history, biology, and treatment of transformed lymphomas". Hematology Am Soc Hematol Educ Program 2009: 532–41. doi:10.1182/asheducation-2009.1.532.PMID 20008238.
23. Martin NE, Ng AK (November 2009). "Good things come in small packages: low-dose radiation as palliation for indolent non-Hodgkin lymphomas". Leuk. Lymphoma 50 (11): 1765–72. doi:10.3109/10428190903186510.PMID 19883306.
24. Kuruvilla J (2009). "Standard therapy of advanced Hodgkin lymphoma". Hematology Am Soc Hematol Educ Program2009: 497–506. doi:10.1182/asheducation-2009.1.497. PMID 20008235.
25. [1] Data from the USA 1999–2006, All Races, Both Sexes: Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK (eds). SEER Cancer Statistics Review, 1975–2007, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER web site, 2010.
26. "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov. 11, 2009.
27. Horner MJ, Ries LAG, Krapcho M, Neyman N, et al. (eds). "SEER Cancer Statistics Review, 1975–2006".Surveillance Epidemiology and End Results (SEER). Bethesda, MD: National Cancer Institute. Retrieved 3 November 2009. "Table 1.4: Age-Adjusted SEER Incidence and U.S. Death Rates and 5-Year Relative Survival Rates By Primary Cancer Site, Sex and Time Period"
28. Hellman, Samuel; Mauch, P.M. Ed. (1999). Hodgkin's Disease. Chapter 1: Lippincott Williams & Wilkins. p. 5.ISBN 0-7817-1502-4.
29. Feller, Alfred C.; Diebold, Jacques (2004). Histopathology of Nodal and Extranodal Non-Hodgkin's Lymphomas(3rd ed.). Springer. ISBN 978-3-540-63801-8.
30. http://www.clinicaltrials.gov/ct2/results?term=lymphoma
31. "Understanding Clinical Trials for Blood Cancers". Leukemia and Lymphoma Society. Retrieved 19 May 2010.