Hepatocellular carcinoma (HCC) is one of the most common malignant tumors. Due to its insidious onset, over half of HCC patients are already in the advanced stage at the time of diagnosis. About 75% of HCC cases occur in Asia, with China accounting for over 50% of the global burden. Among them, in Asia, especially in China where the incidence of advanced HCC is highest, newly diagnosed liver cancer tumors often involve major vascular invasion (MVI), which is more common compared to extrahepatic metastasis (EHS).
However, so far, there is still no consensus or guideline specifically for the treatment of locally advanced HCC, especially in the population involving high tumor burden within the liver and accompanying MVI. Is there an effective and safe treatment method for these patients? Recently, Dr. Long Xin'an from Fuda Cancer Hospital shared insights on the treatment of primary liver cancer with HAIC.

01 What is HAIC?
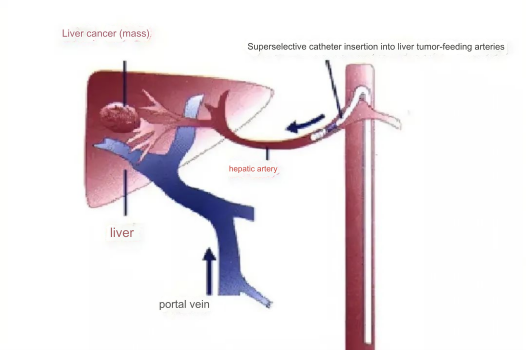
HAIC, namely Hepatic Arterial Infusion Chemotherapy, is a treatment method that delivers chemotherapy drugs directly into the tumor-feeding arteries via the hepatic artery, increasing the local concentration of drugs in the lesions. It effectively reduces tumor burden while mitigating systemic toxicity through the first-pass elimination effect of the liver.
Since 1995, the HCC guidelines of the Japanese Society of Hepatology have listed HAIC as an effective treatment for locally advanced HCC. In the HCC guidelines of South Korea, HAIC is recommended for advanced HCC patients without EHS, who have failed systemic treatment or are not suitable for systemic treatment. In the HCC consensus guidelines of Taiwan, China, HAIC is also recommended as the preferred treatment option for patients with portal vein tumor thrombus (PVTT).
Currently, HAIC has become an important treatment method for middle and late-stage liver cancer and is included in the "Diagnosis and Treatment Guidelines for Primary Liver Cancer (2022 edition)" by the National Health Commission of China. In addition, the Chinese Society of Clinical Oncology recommends HAIC-FOLFOX (a chemotherapy regimen combining oxaliplatin, calcium folinate, and fluorouracil) as one of the optional treatment options for advanced HCC patients. Increasing evidence suggests that HAIC is an effective treatment for HCC.
02 How is HAIC performed?
The operation method of HAIC is similar to that of conventional transarterial chemoembolization (TACE). Firstly, the right femoral artery (or other arteries such as the radial artery, subclavian artery, etc.) is punctured, and a catheter is inserted and respectively placed in the celiac trunk and superior mesenteric artery for angiography. According to the tumor's arterial blood supply, the catheter is selectively placed in the tumor-feeding artery. If the tumor receives blood supply from both the celiac trunk and superior mesenteric artery or from other sources, the microcatheter is placed in the largest tumor-feeding artery.
During HAIC treatment, microcatheters with or without port implantable catheter systems are commonly used for FOLFOX therapy. Currently, repeated single-dose administration of FOLFOX is the preferred arterial infusion technique in clinical practice. If no significant disease progression is observed in the initial follow-up assessment, it is recommended to continue HAIC treatment for at least 4 cycles. If there is progression of extrahepatic lesions while intrahepatic lesions are controlled, systemic treatment should be combined with HAIC. If there is significant progression of intrahepatic lesions or intolerable toxic reactions, discontinuation of HAIC treatment should be considered.
It is worth noting that the effectiveness of HAIC treatment depends on the selected infusion drug regimen. In HAIC treatment based on oxaliplatin, the most commonly used treatment regimens include single-agent HAIC-FOLFOX, HAIC combined with molecular targeted agents (MTAs), HAIC combined with immune checkpoint inhibitors (ICIs), triple therapy of HAIC combined with ICIs and MTAs, and HAIC combined with TACE.
Due to the heterogeneity of tumors, there is a significant difference in the sensitivity of advanced HCC patients to chemotherapy. To maximize the survival benefit of the entire patient population, potential responders to HAIC-FOLFOX treatment can be screened through predictive means, and potential non-responders should be switched to other effective treatment options as early as possible. However, whether to perform HAIC still requires specific evaluation of individual cases by doctors.
03 Who is suitable for HAIC?
HAIC treatment is usually suitable for HCC patients with high tumor burden within the liver. However, for patients with few extrahepatic metastases, when intrahepatic tumor burden or liver function is the primary prognostic factor, HAIC is also one of the optional treatment methods. In recent clinical trials on HAIC-FOLFOX, patients with compensated liver function of Child-Pugh A to B7 grades showed good tolerance to single-agent HAIC treatment or combined HAIC with systemic treatment. In addition, HAIC treatment can be used perioperatively as adjuvant therapy to reduce the risk of recurrence in HCC patients and improve surgical outcomes.
04 Complications and Management of HAIC
Thrombosis leading to catheter occlusion or dislocation of the catheter tip: Heparin injection can prevent thrombosis after catheter placement. Once catheter occlusion is confirmed, the catheter should be replaced. If catheter tip dislocation is found, the patient should be transferred to the DSA operating room for catheter repositioning. In addition, attention should be paid to gentle and standardized puncture and catheter placement to avoid vascular complications (such as stenosis, occlusion, and pseudoaneurysm), and anticoagulants such as rivaroxaban may be used if necessary.
Abdominal pain: It may be related to rapid tumor shrinkage or arterial spasm caused by oxaliplatin infusion. Generally, this pain mostly occurs during oxaliplatin infusion and quickly subsides after infusion. However, in a small number of patients, this pain may be more severe, but it can be quickly relieved by suspending oxaliplatin infusion or symptomatic treatment (such as lidocaine analgesia and papaverine to relieve spasms).
Chemotherapy-related toxicity of HAIC treatment itself: Common adverse events (AEs) include thrombocytopenia, neutropenia, vomiting, diarrhea, liver function impairment (such as elevated ALT, AST, and total bilirubin), renal function impairment (such as elevated creatinine), and other complications related to combined drug use, such as hand-foot syndrome and hypertension. The drug-related complications of HAIC-EOIFOX treatment are mostly tolerable and can be relieved by symptomatic treatment.
The recommended principles for managing adverse reactions related to HAIC are as follows: for grade 1-2 AEs, symptomatic treatment without dose adjustment; for grade 3 or 4 AEs, infusion should be stopped appropriately, and symptomatic treatment should be given actively. The chemotherapy drug dose in the next course should be adjusted according to the situation, and HAIC treatment should be stopped promptly if necessary.

HAIC has a positive therapeutic effect on advanced HCC and may be one of the salvage treatment options after other treatments are ineffective or fail. However, HAIC treatment faces issues such as hepatic artery catheterization technology and standardization of the optimal treatment regimen. In the future, HAIC will be further explored in combination with standardized treatment, ablation therapy, molecular targeted therapy, and immunotherapy.