Esophageal cancer (or oesophageal cancer) is malignancy of the esophagus. There are various subtypes, primarily squamous cell cancer (approx 90–95% of all esophageal cancer worldwide) and adenocarcinoma (approx. 50–80% of all esophageal cancer in the United States). Squamous cell cancer arises from the cells that line the upper part of the esophagus. Adenocarcinoma arises from glandular cells that are present at the junction of the esophagus and stomach.[1]
Esophageal tumors usually lead to dysphagia (difficulty swallowing), pain and other symptoms, and are diagnosed with biopsy. Small and localized tumors are treated surgically with curative intent. Larger tumors tend not to be operable and hence are treated with palliative care; their growth can still be delayed with chemotherapy, radiotherapy or a combination of the two. In some cases chemo- and radiotherapy can render these larger tumors operable. Prognosis depends on the extent of the disease and other medical problems, but is generally fairly poor.

Classification
Esophageal cancers are typically carcinomas which arise from the epithelium, or surface lining, of the esophagus. Most esophageal cancers fall into one of two classes: squamous cell carcinomas, which are similar to head and neck cancer in their appearance and association with tobacco and alcohol consumption, and adenocarcinomas, which are often associated with a history of gastroesophageal reflux disease and Barrett's esophagus. A general rule of thumb is that a cancer in the upper two-thirds is a squamous cell carcinoma and one in the lower one-third is an adenocarcinoma. Rare histologic types of esophageal cancer are different variants of the squamous cell carcinoma, and non-epithelial tumors, such asleiomyosarcoma, malignant melanoma, rhabdomyosarcoma, lymphoma and others.[3][4]
Signs and symptoms
Dysphagia (difficulty swallowing) and odynophagia (painful swallowing) are the most common symptoms of esophageal cancer. Dysphagia is the first symptom in most patients. Odynophagia may also be present. Fluids and soft foods are usually tolerated, while hard or bulky substances (such as bread or meat) cause much more difficulty. Substantial weight loss is characteristic as a result of reduced appetite, poor nutrition and the active cancer. Pain behind the sternum or in theepigastrium, often of a burning, heartburn-like nature, may be severe, present itself almost daily, and is worsened by swallowing any form of food. Another sign may be an unusually husky, raspy, or hoarse-sounding cough, a result of the tumor affecting the recurrent laryngeal nerve.
The presence of the tumor may disrupt normal peristalsis (the organized swallowing reflex), leading to nausea and vomiting, regurgitation of food, coughing and an increased risk of aspiration pneumonia. The tumor surface may be fragile and bleed, causing hematemesis (vomiting up blood). Compression of local structures occurs in advanced disease, leading to such problems as upper airway obstruction and superior vena cava syndrome. Fistulas may develop between the esophagus and thetrachea, increasing the pneumonia risk; this condition is usually heralded by cough, fever or aspiration.[2]
Most of the people diagnosed with esophageal cancer have late-stage disease, because people usually do not have significant symptoms until half of the inside of the esophagus, called the lumen, is obstructed, by which point the tumor is fairly large. [5]
If the disease has spread elsewhere, this may lead to symptoms related to this: liver metastasis could cause jaundice and ascites, lung metastasis could cause shortness of breath, pleural effusions, etc.
Causes
Increased risk
There are a number of risk factors for esophageal cancer.[2] Some subtypes of cancer are linked to particular risk factors:
-Age – most patients are over 60, and the median in US patients is 67.[2]
-Sex – the disease is more common in men.
-Heredity – it is more likely in people who have close relatives with cancer.
-Tobacco smoking and heavy alcohol use increase the risk, and together appear to increase the risk more than either individually. Tobacco and alcohol account for approximately 90% of all esophageal squamous cell carcinomas. Tobacco smoking is also linked to esophageal adenocarcinoma though no scientific evidence has been found between alcohol and esophageal adenocarcinoma.[6]
-Gastroesophageal reflux disease (GERD) and its resultant Barrett's esophagus increase esophageal cancer risk due to the chronic irritation of the mucosal lining. Adenocarcinoma is more common in this condition.[7] A consequence of GERD is increased exposure of the esophagus to bile acids; and bile acids have been implicated as causal agents in esophageal adenocarcinoma (reviewed by Bernstein et al.)[8]
-Human papillomavirus (HPV)[9]
-Corrosive injury to the esophagus by swallowing strong alkalines (lye) or acids
-Particular dietary substances, such as nitrosamines
-A medical history of other head and neck cancers increases the chance of developing a second cancer in the head and neck area, including esophageal cancer.
-Plummer–Vinson syndrome (anemia and esophageal webbing)
-Tylosis and Howel–Evans syndrome (hereditary thickening of the skin of the palms and soles)
-Radiation therapy for other conditions in the mediastinum[2]
-Coeliac disease predisposes towards squamous cell carcinoma.[10]
-Obesity increases the risk of adenocarcinoma fourfold.[11] It is suspected that increased risk of reflux may be behind this association.[7][12]
-Thermal injury as a result of drinking hot beverages[13][14]
-Alcohol consumption in individuals predisposed to alcohol flush reaction[15]
-Achalasia[16]
Decreased risk
-Risk appears to be less in patients using aspirin or related drugs (NSAIDs).[17]
-The role of Helicobacter pylori in progression to esophageal adenocarcinoma is still uncertain, but, on the basis of population data, it may carry a protective effect.[18][19] It is postulated that H. pylori induces chronic gastritis, which is a risk factor for reflux, which in turn is a risk factor for esophageal adenocarcinoma.[20]
-According to the National Cancer Institute, "diets high in cruciferous (cabbage, broccoli/broccolini, cauliflower, Brussels sprouts) and green and yellow vegetables and fruits are associated with a decreased risk of esophageal cancer."[21]
-Moderate coffee consumption is associated with a decreased risk.[22]
-According to one Italian study of "diet surveys completed by 5,500 Italians"—a study which has raised debates questioning its claims among cancer researchers cited in news reports about it—eating pizza more than once a week appears "to be a favorable indicator of risk for digestive tract neoplasms in this population."[23]
Diagnosis
Clinical evaluation
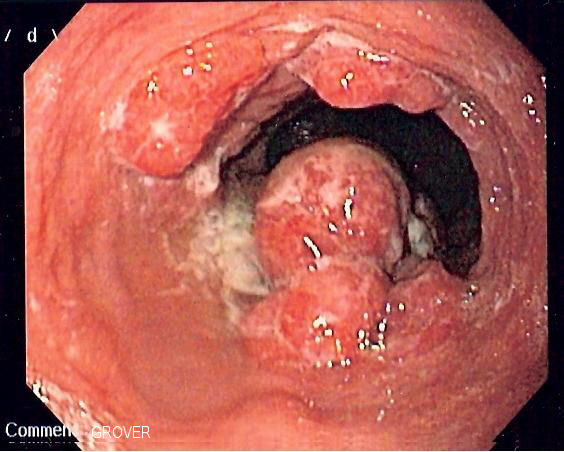
Although an occlusive tumor may be suspected on a barium swallow or barium meal, the diagnosis is best made with esophagogastroduodenoscopy (EGD, endoscopy); this involves the passing of a flexible tube down the esophagus and examining the wall. Biopsies taken of suspicious lesions are then examined histologically for signs of malignancy.
Additional testing is usually performed to estimate the tumor stage. Computed tomography (CT) of the chest, abdomen and pelvis can evaluate whether the cancer has spread to adjacent tissues or distant organs (especially liver and lymph nodes). The sensitivity of a CT scan is limited by its ability to detect masses (e.g. enlarged lymph nodes or involved organs) generally larger than 1 cm. Positron emission tomography is also used to estimate the extent of the disease and is regarded more precise than CT alone. Esophageal endoscopic ultrasound can provide staging information regarding the level of tumor invasion, and possible spread to regional lymph nodes.
The location of the tumor is generally measured by the distance from the teeth. The esophagus (25 cm or 10 inches long) is commonly divided into three parts for purposes of determining the location. Adenocarcinomas tend to occur distally and squamous cell carcinomas proximally, but the converse may also be the case.